0691
4D flow MRI Improves Dissection Flap Fenestration Detection in Type B Aorta Dissection1Radiology, Northwestern University, Chicago, IL, United States, 2Biomedical Engineering, Northwestern University, Chicago, IL, United States
Synopsis
Type B aortic dissections involve the aortic arch/descending aorta with false lumen patency/thrombosis, and size of entry tears identified as predictors of adverse events. These parameters suggest a complex hemodynamic environment that is poorly assessed by current diagnostic tools. The presence of additional fenestrations in the dissection flap likely also alters false lumen hemodynamics. 4D flow MRI offers a comprehensive assessment of 3D aortic hemodynamics in type B dissection. Our results demonstrate that 4D flow can detect nearly two-times the number of dissection flap fenestrations relative to time-resolved MRA, suggesting the potential for improved hemodynamic characterization of these patients.
Introduction
Aortic dissections are caused by a tear of the aortic wall intima creating a low-flow false lumen and a true lumen for continued blood flow peripherally, with lumens separated by a dissection flap. Type B aortic dissections involve the aortic arch/descending aorta and can result 5-year mortality rates of ~20%.(1) Previous work has demonstrated that descending aorta size, false lumen patency/thrombosis, and size of entry tears (connections between true and false lumen) are important predictors of adverse events such as rupture in type B dissection patients.(2) The reliable identification of entry tears and associated flow jets entering and exiting the false lumen is critical for understanding complex dissection hemodynamics and pressure in the false lumen.
Current diagnostic tools such as CT angiography, MR angiography (MRA), and time-resolved MRA (TRMRA) are limited in their ability to detect small tears and offer minimal information on entry/exit flow and true and false lumen hemodynamics. 4D flow MRI offers a comprehensive assessment of 3D aortic hemodynamics in type B dissection (3), and there are now commercially available tools for easy and efficient visualization of these image data sets. Beyond entry and exit tears, the presence of additional fenestrations in the dissection flap likely alters false lumen hemodynamics, and diastolic retrograde flow (false to true lumen) through these defects may indicate elevated false lumen pressures. These findings have the potential to impact surgical approach and risk-stratification. In the current study, we compare fenestration dissection flap fenestration visualization between 4D flow MRI and TRMRA.
Methods
Nine patients with type B dissections (age: 57±5 years, 5 men, 4 women) were retrospectively identified from a cohort of patients who had undergone standard-of-care MRA of the chest which included aortic 4D flow MRI. Four of these patients had previous type A (ascending aorta) dissection repairs, and one patient had a previous type B repair with persistent dissection. TRMRA were acquired in the LAO orientation with spatial resolution = 1.3x0.9 mm2 and temporal resolution = 2.4 sec. 4D flow images were acquired using prospective ECG and respiratory navigator gating with an imaging volume covering the entire thoracic aorta in the left anterior oblique orientation. Pulse sequence parameters were: spatial resolution = 2.3x3.0x2.5 mm3, temporal resolution = 40 ms, velocity sensitivity = 150 cm/s. 4D flow images were post-processed and visualized on dedicated software (cvi42, Circle Cardiovascular Imaging, Inc, Canada). Cine 4D flow velocity maximum intensity projection (MIP) images were qualitatively evaluated by a radiologist with the ability to pan, zoom, and rotate images, and change the velocity color scale to optimize visualization. Images were evaluated qualitatively true and false dissection lumen detection, dissection flap fenestrations count, and qualitative assessment of retrograde flow through the fenestrations. Entry and exit tears were counted as fenestrations. TRMRA was presented in the standard clinical fashion as a MIP in the LAO projection in a different reading session, and assessed on the same quality metrics as 4D flow MRI. The numbers of fenestrations were compared between 4D flow and TRMRA using a χ2-test and alpha of 0.05.Results
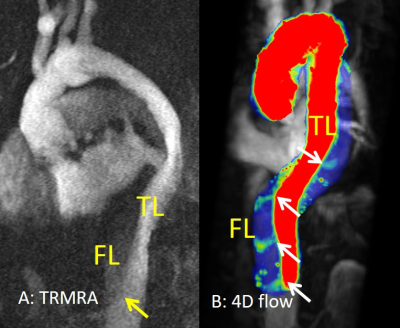
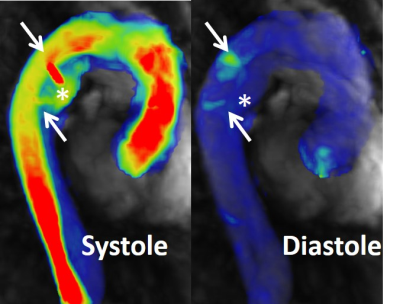
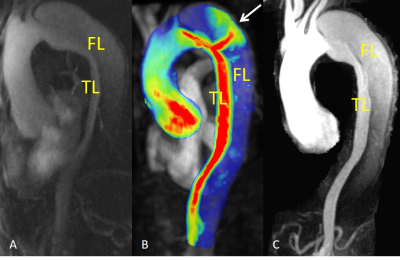
Using 4D flow MRI, true and false lumens were clearly visualized in all nine patients. A total of 20 fenestrations were identified (Figure 1), and 14 of these fenestrations demonstrated retrograde flow from the false lumen to true lumen during diastole (Figure 2). Seven patients had concurrently performed TRMRA, and true and false lumens were visualized in all patients (Figure 3). In these patients, 4D flow identified nearly twice as many fenestrations (4D flow: 15 fenestrations, TRMRA: 8 fenestrations, p = 0.002). Retrograde flow through fenestrations could not be seen on any TRMRA. The ability to visualize fenestrations on TRMRA was limited to observing early filling of the false lumen, while visualizing fenestrations on 4D flow MRI was aided by the ability to rotate the images, see isolated flow jets, and visualize retrograde jets during diastole.Conclusions
4D flow MRI in chronic type B dissections patients is superior to TRMRA for the detection of small dissection flap fenestrations. Moreover, observing the flow throughout the cardiac cycle allows for identification of retrograde flow through these small fenestrations from the false to true lumen. Overall, when viewed on an appropriate workstation with the ability to pan, zoom, and rotate the images, 4D flow MRI provides superior qualitative type B aorta dissection hemodynamic assessment. Future work will focus on correlating fenestration count and location with false lumen thrombosis and propagation, as well as quantitative assessment of flow dynamics in the true and false lumens and through the fenestration defects.Acknowledgements
No acknowledgement found.References
1. Goldfinger JZ, Halperin JL, Marin ML, Stewart AS, Eagle KA, Fuster V. Thoracic aortic aneurysm and dissection. J Am Coll Cardiol 2014;64(16):1725-1739.
2. Evangelista A, Salas A, Ribera A, et al. <span hwp:id="article-title-1" class="article-title">Long-Term Outcome of Aortic Dissection With Patent False Lumen</span><span hwp:id="article-title-39" class="sub-article-title">Clinical Perspective</span>. Predictive Role of Entry Tear Size and Location 2012;125(25):3133-3141.
3. Clough RE, Waltham M, Giese D, Taylor PR, Schaeffter T. A new imaging method for assessment of aortic dissection using four-dimensional phase contrast magnetic resonance imaging. J Vasc Surg 2012;55(4):914-923.
Figures