0612
Assessment of Portal Hypertension with Multi-parametric Hepatic MR Elastography in Mouse Models1Radiology, Mayo Clinic, Rochester, MN, United States, 2Gastroenterology and Hepatology, Mayo Clinic, Rochester, MN, United States
Synopsis
We used multi-parametric hepatic MR Elastography (MRE) in two different mouse models with congestion and cirrhosis-induced portal hypertension, respectively. Spearman correlation was used to analyze the relationships between the MRE-assessed liver stiffness, damping ratio, volumetric strain, stiffness frequency dispersion, and the portal pressure directly measuared in vivo. We found that volumetric strain and damping ratio had negative correlations (ρ=-0.7515, ρ=-0.5528 respectively), while shear stiffness had a positive correlation (ρ=0.6983) with portal pressure. Additionally, damping ratio changes differently in portal hypertension induced by congestion and cirrhosis. In summary, multi-parametric MRE has potential to differentiate and quantify congestion and cirrhosis-induced portal hypertension.
Introduction
Portal hypertension (PHT), an increase in the pressure gradient between the portal vein and the inferior vena cava, is associated with high mortality in patients with chronic liver diseases. Nowadays, the gold standard for assessing PHT is the transvenously invasive measurement of the hepatic venous pressure gradient (HVPG), which has a potential bias for presinusoidal abnormalities, such as primary biliary cirrhosis1,2. Some studies have shown the sensitivity of volumetric strain to detect tissue pressure change in an excised sheep liver and also patients with PHT3. Investigators have also found that shear stiffness and damping ratio vary differently with respect to causes of PHT4. We hypothesized that the multiple parameters calculated from 3D MRE images can distinguish different mechanical responses caused by increased fluid volume pressure in soft tissues. Thus, the purpose of our study is to apply multi-parametric hepatic MRE to validate the usefulness of MRE parameters, including volumetric strain, shear stiffness, damping ratio, and stiffness frequency dispersion, for predicting PHT in two different mouse models.Methods
We studied 32 wild-type male mice, including 16 mice with congestion-induced PHT by partial inferior vena cava ligation (pIVCL)5, 5 mice with cirrhosis-induced PHT by bile duct ligation (BDL), and 11 mice with sham surgery as age-matched controls. All experiments were implemented on a 3.0-T GE imager with a custom 4-cm birdcage multi-channel coil. A silver needle was used to generate shear waves throughout the liver, which were anesthetized with 1.0-1.5% isoflurane. We performed 3D EPI-MRE of the liver from 80 to 400Hz (Figure 1), with a resolution of 0.3×0.3×2mm3. The ROIs were drawn to encompass as much of the liver as possible that had significant wave propagation while excluding the vibrating source and adjacent area. Multiple MRE parameters were calculated. We measured the portal pressure by introducing a pressure sensor in the portal vein before animal sacrificing, and used whole liver specimens for quantifying the hydroxyproline concentration. Spearman correlations were used to analyze the relationships between the MRE parameters and portal pressure. A significance level of P<0.05 was used in this study, correlation coefficient (ρ) greater than 0.5 was considered good.Results
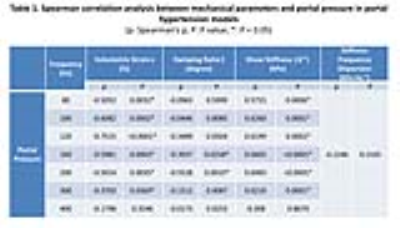
Figure 1 demonstrates example MRE wave images obtained in one of the controls. The mean portal pressure increased significantly in both models, compared with the controls (P<0.05), as shown in Figure 2. The BDL model had significant fibrosis (P<0.05), while there was only mild fibrosis in pIVCL mice at 6 weeks after surgery. Table 1 and Figure 3 illustrate that volumetric strain (120Hz) and damping ratio (200Hz) had negative correlations with portal pressure (ρ=-0.7515, P<0.0001*; ρ=-0.5528, P=0.0010*), while the shear stiffness (200Hz) had positive correlation (ρ=0.6983, P<0.0001*). However, the stiffness frequency dispersion wasn’t correlated with portal pressure (P=0.2165). Figure 4 shows that the mean volumetric strain (120Hz) of pIVCL mice at 6 weeks (0.33%±0.03%), was similar to that of BDL mice (0.34%±0.03%), which corresponds with changes of portal pressure (6.58±0.73mmHg, 6.26±0.90mmHg respectively), while the mean damping ratio (200Hz) varied much more (0.038±0.014 vs. 0.027±0.012, respectively).Discussion
This study investigated the assessment of PHT with multi-parametric hepatic MRE in two mouse models, both congestion- and cirrhosis-induced PHT. When the PHT progressively increased, volumetric strain and damping ratio decreased, while shear stiffness increased. The volumetric strain and damping ratio, which are derived from compressional and shear wave fields respectively, may reflect mechanical responses of soft tissue that experience varying etiology with fluid pressure/volume changes. We believe that decreased volumetric strain may represent increased vascular/tissue pressure in PHT, while the elevated damping ratio mainly reflects composite change caused by interstitial fluid volume augmentation in hepatic inflammation or edema. The damping ratio increased significantly in pIVCL mice at 6 weeks, maybe because the onset of liver injury and subsequent fibrosis developed at that time. As for BDL model, it was lower, reflecting that damping ratio increased at the early onset of liver fibrosis, but was not able to detect moderate and severe liver injury, which was similar to previous studies4. Since we only have 5 mice in BDL group and the control was calculated as the mean value of all sham groups, the changes were not significant. However, as an ongoing study, by the time of the presentation, we will have more data.Conclusion
Our preliminary results suggest that multi-parametric MRE can quantify PHT with volumetric strain and distinguish the causes of PHT using the damping ratio. We believe that more data from these two PHT models will further cross-validate the usefulness of multi-parametric MRE in early recognition and precise diagnosis of PHT.Acknowledgements
This research was funded by NIBIB grants EB017197 (M.Y) and EB001981 (R.L.M)References
1. Vorobioff JD. Hepatic venous pressure in practice: how, when, and why. J Clin Gastroenterol. 2007;41(Suppl 3):S336–343.
2. Annalisa B. Assessing portal hypertension in liver diseases. Expert Review of Gastroenterology & Hepatology. 2013;7(2):141-155.
3. Sebastian H. Towards Compression-Sensitive Magnetic Resonance Elastography of the Liver: Sensitivity of Harmonic Volumetric Strain to Portal Hypertension. Journal of Magnetic Resonance Imaging. 2014;39:298-306.
4. Meng Y. Distinguishing between Hepatic Inflammation and Fibrosis with MR Elastography. Radiology. 2017;284(3):694-705.
5. Douglas A. Simonetto. Chronic Passive Venous Congestion Drives Hepatic Fibrogenesis Via Sinusoidal Thrombosis and Mechanical Forces. Hepatology. 2015;61:648-659
Figures