0600
MRI-guided right heart catheterization using a commercial nitinol guidewire: Experience in 6 patients1National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD, United States
Synopsis
We have performed MRI-guided right heart catheterization in patients with a commercial nitinol guidewire for the first time. MRI-guided cardiovascular interventions have been limited by the unavailability of an guidewire that is safe and visible. Here, we use real-time spiral gradient echo imaging to reduce RF-induced heating on a commercial nitinol 150cm Glidewire. The Glidewire was found to generate <0.2°C in the ASTM-2182 phantom in all configurations. With IRB approval, the guidewire catheterization was performed on six patients. Blood biomarkers remained normal and the reported clinical benefits were increased shaft conspicuity, increased shaft stiffness, and ability to track to chambers.
Introduction
The scope of cardiovascular procedures performed under MRI-guidance has been limited by the unavailability of a visible and safe guidewire for the MRI scanner. Standard commercial nitinol guidewires have not been useable in the MRI scanner due to concerns of RF-induced heating. Previous efforts to design safer active and passive devices specifically for MRI-guided procedures have generated few commercial devices. We have previously shown that by using spiral gradient echo imaging with reduced RF power and duty cycle for image acquisition, we can mitigate the RF-induced heating of nitinol guidewires [1]. Here, we report the use of a nitinol Glidewire for MRI-guided right heart catheterization in six patients.Methods
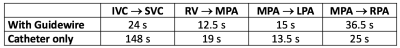
This study was approved the National Heart, Lung, and Blood Institute’s Institutional Review Board. Heating of 0.035” commercial guidewires was assessed in the ASTM-2182 phantom in a range of configurations in order to prove safety. For our clinical study, we used the 150cm angled tip nitinol Glidewire (Terumo, Tokyo, Japan). We performed MRI-guided right heart catheterization on 6 clinical patients using the nitinol Glidewire and a “T” tip balloon wedge catheter (Edwards, Irvine, CA) with gadolinium- or air-filled balloon. The guidewire was used to navigate from inferior vena cava (IVC) to superior vena cava (SVC) and to navigate the pulmonary vasculature. The time required to navigate from IVC to SVC, from right ventricle (RV) to main pulmonary artery (MPA), MPA to right pulmonary artery (RPA) and MPA to left pulmonary artery (LPA) were recorded with a guidewire (n = 6) and balloon catheter alone (n = 3). Following the procedure, D-dimer and serum free hemoglobin were measured from paired blood samples taken immediately before and after the procedure.
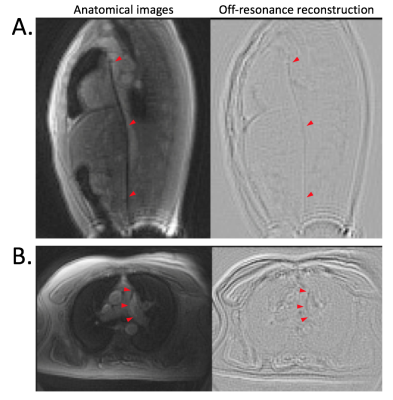
Real-time imaging was performed on a 1.5T system (Aera, Siemens Healthcare, Erlangen, Germany) with spiral gradient echo imaging (16 interleaves, TE/TR = 0.82ms/10ms, FOV = 400mm, slice thickness = 8mm, flip angle = 10°). Gadolinium-filled balloon visibility was improved using a partial saturation pulse with flip angle = 45° [2]. Difference images from reconstructions of the spiral data at ± 100Hz were used to enhance off-resonance for improved guidewire visibility [3]. During the procedure, both standard anatomical images and off-resonance enhanced images were displayed simultaneously to operating physicians.
Results
This Glidewire generated <0.2°C in the ASTM-2182 gel phantom in all configurations during real-time spiral gradient echo imaging, with less heating in vivo because of the central position of vessels and blood flow cooling.
A diagnostic right-heart catheterization was successfully completed in all 6 patients and blood thermal injury biomarkers were normal following the guidewire catheterization. The average time required for each procedural stage is given in Figure 1. Time to enter the SVC was improved with the guidewire, and time to navigate the pulmonary vasculature remained similar. In one patient, the LPA was only accessible using a guidewire.
The primary clinical benefit reported by operators was increased shaft conspicuity, increased shaft stiffness, and ability to track to chambers such as LPA. Figure 2A shows improved catheter shaft conspicuity in the SVC created by the guidewire. Figure 2B shows the guidewire engaging the LPA with visible guidewire shaft. The gadolinium- or air-filled balloon catheter tip was conspicuous, but the guidewire tip had limited visibility.
Discussion
Image quality and blood-myocardial contrast was inferior using the spiral gradient echo imaging compared with standard real-time bSSFP used for MRI-guided right heart catheterization. However, clinicians preferred the trade-off in image quality for enhanced catheter performance and conspicuity. This specific Glidewire model is fully insulated and does not contain coils for radio-opacity, making it less susceptible to RF-induced heating compared with other commercial guidewires tested. Improved guidewire tip conspicuity will be required for procedures in the left-heart.Conclusion
This first-in-human study used gradient echo spiral imaging to safely perform MRI-guided right heart catheterization with an off-the-shelf metallic guidewire from the catheterization lab. These RF-efficient imaging methods may have the potential to enable more MRI-guided procedures using commercial metallic devices in the future.Acknowledgements
This work was supported by the NHLBI DIR (Z01-HL006039, Z01-HL005062, ZIA-HL006213).References
[1] Campbell-Washburn AE, Rogers T, Basar B, Sonmez M, Kocaturk O, Lederman RJ, Hansen MS and Faranesh AZ. Positive contrast spiral imaging of a nitinol guidewire with reduced RF-induced heating. Journal of Cardiovascular Magnetic Resonance (2015), 17:114 .
[2] Velasco Forte MN, Pushparajah K, Schaeffter T, Perez IV, Rhode K, Ruijsink B, Alhrishy M, Byrne N, Chiribiri A, Ismail T, Hussain T, Razavi R and Roujol S. Improved passive catheter tracking with positive contrast for CMR-guided cardiac catheterization using partial saturation (pSAT). Journal of Cardiovascular Magnetic Resonance (2017) 19:60.
[3] Campbell-Washburn AE, Basar B, Rogers T, Sonmez M, Kocaturk O, Lederman RJ, Hansen MS and Faranesh AZ. Two-channel visualization of a passive nitinol guidewire with iron oxide maker created from a single image acquisition. Proceedings of the 23rd annual meeting of the ISMRM (Toronto 2015): 0868.
Figures