0599
Initial results for MRI-guided catheterization in children and young adults with congenital heart disease using the partial saturation (pSAT) sequence1Division of Imaging Sciences and Biomedical Engineering, King's College London, London, United Kingdom, 2Paediatric Cardiology, Queen Elizabeth University Hospital, Glasgow, United Kingdom, 3Division of Imaging and Biomedical Engineering, King's College London, London, United Kingdom, 4King's College London, London, United Kingdom, 5Philips, Hamburg, Germany, 6Physikalisch-Technische Bundesanstalt, Berlin, Germany, 7Philips Research Laboratories, Hamburg, Germany, 8UT Southwestern Medical Center, Dallas, TX, United States
Synopsis
CMR is a promising alternative to x-ray fluoroscopy for the guidance of cardiac catheterization procedures. We have recently developed a partial saturation (pSAT) sequence which enables passive tracking of balloon-wedge catheters with positive contrast, using a dilution containing gadolinium. 23 patients from 2 different centres were recruited. MRI-guidance was performed using the pSAT sequence applied in the iSuite platform® or an interactive imaging mode. During real-time MRI catheterization the balloon was visualized during 64±19% of the scanning time. pSAT angle was 30-50° in all patients. Mean subjective image quality scores were 3.7 out of 5 for heart visualisation and 4.6/5 for balloon/blood contrast.
Introduction:
In the last decades, there has been an increase in the prevalence of adults with complex CHD. Cardiac catheterization is a common technique used for the clinical management of these patients, usually guided by X-ray fluoroscopy. However, a recent study has shown a significant raise in biomarkers of chromosomal damage following diagnostic and therapeutic cardiac catheterization procedures, stating that no safe dose exists for radiation in children (1). The feasibility of MRI-guided cardiac catheterization has been demonstrated in patients, avoiding or minimizing radiation (2) (3). We have recently developed a technique based on partial saturation (pSAT) which enables simultaneous visualization of the catheter tip and the cardiovascular anatomy (4). In this study, we evaluated its performance for diagnostic MRI-guided catheterization in children and young adults with congenital heart disease in two different centres.
Methods:
23 consecutive patients were referred for MRI-guided catheterization for pulmonary vascular resistance (PVR) analysis. Four patients could not be recruited, 16 were enrolled at our institutions and imaged using an XMR system and 3 patients were recruited at a different centre. Our hybrid laboratory is configured by a 1.5T Philips Achieva combined BV Pulsera cardiac X-Ray unit); the external centre used a 1.5T Philips Ingenia MRI system. MRI-guidance was performed using the pSAT sequence with the iSuite real-time visualization platform® or an interactive imaging mode in the scanner console. Slice thickness and pSAT angle were the main factors adapted to run the sequence in each case. PVR analysis was recorded. Radiation dose and time, duration of catheterization under MRI-guidance and adverse events were reported. Fraction of time when the catheter tip was visible during real-time MRI imaging was also evaluated. Visualization of the heart anatomy and catheter balloon/blood contrast were scored by 3 MRI-catheterisation experts from both institutions. All images received two scores involving anatomical visualization and contrast between the cardiac structures and the balloon at the tip of the catheter (1-poor; 5-excellent) (4).Results:
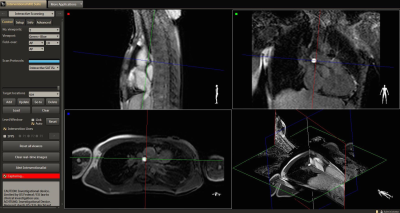
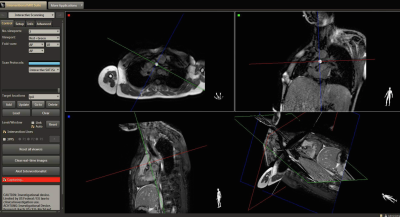
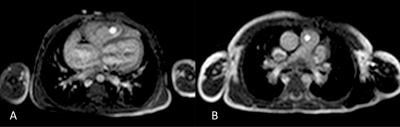
19 patients were recruited for the study (42% females). Median age and weight were 3.5 years (range: 2 months-39 years) and19 kg (range: 5-98), respectively. After initial evaluation, MRI guidance was not attempted in two patients, owing to the need of wire in one case and clinical instability in a different patient. Of the remaining 17 patients, 37% underwent right heart catheterization (Figure 1), 42% underwent both left and right catheterization and 21% had single ventricle circulation (Figure 2). In our centre, iSuite® platform was used in 12 patients. In 5 (3 from external centre), the pSAT sequence was used in interactive mode in the scanner (Figure 3). In 4 patients, the procedure was performed solely under MRI guidance, 3 Fontan patients had >50% performed under MRI. For the remaining cases a stiffer catheter and/or a wire with the subsequent need for x-ray support was required. There was a significant trend towards needing x-ray guidance compared to MRI in smaller patients. pSAT angle was 30-50° in all patients, slice thickness was 5-10 mm. Mean subjective image quality scores varied from 3.7±0.96 for heart visualisation and 4.6±0.6 for balloon/blood contrast. Visualization of the balloon at the tip of the catheter was achieved in all the studies. During real-time MRI catheterization the balloon was visualized during 64±19% of the scanning time. Median radiation time and dose were 11 min (range: 0-52) and 0.3 mGy.m2 (range: 0-2.8), respectively. Mean catheterization time under MRI was 34±23 min.Discussion:
Visualization of the catheter tip and
cardiovascular anatomy during diagnostic interventions was good to excellent during
most of the procedures when using our pSAT sequence (4),
allowing the operator to safely performed diagnostic procedures. However, young
patients with low weight were only partially
catheterized under MRI guidance. This is related to several reasons. First, the
size of the catheter normally used for these patients is 4Fr; these catheters
are less stiff and the balloon at the tip becomes heavier when filled in with a
dilution of gadolinium, becoming more difficult to navigate inside small
structures without the support of a guide-wire. Second, the location of the
patient inside the MRI scanner makes it difficult for the operator to reach the
groin and manipulate the catheter. Conclusions:
MRI-guided catheterization with simultaneous
visualization of the catheter and cardiac anatomy using the pSAT sequence is
feasible in patients with CHD. However, there remains a need for MRI-compatible
guide-wires to enable cardiac catheterisation under MRI-guidance alone in paediatric
patients with complex anatomy.Acknowledgements
N/AReferences
1. Harbron RW, Chapple CL, O'Sullivan JJ, Best KE, Berrington de Gonzalez A, Pearce MS. Survival adjusted cancer risks attributable to radiation exposure from cardiac catheterisations in children. Heart. 2017;103(5):341-6.
2. Rogers T, Ratnayaka K, Khan JM, Stine A, Schenke WH, Grant LP, et al. CMR fluoroscopy right heart catheterization for cardiac output and pulmonary vascular resistance: results in 102 patients. J Cardiovasc Magn Reson. 2017;19(1):54.
3. Pushparajah K, Tzifa A, Bell A, Wong JK, Hussain T, Valverde I, et al. Cardiovascular magnetic resonance catheterization derived pulmonary vascular resistance and medium-term outcomes in congenital heart disease. J Cardiovasc Magn Reson. 2015;17:28. 4. Velasco Forte MN, Pushparajah K, Schaeffter T, Valverde Perez I, Rhode K, Ruijsink B, et al. Improved passive catheter tracking with positive contrast for CMR-guided cardiac catheterization using partial saturation (pSAT). Journal of Cardiovascular Magnetic Resonance. 2017;19(1):60.
Figures