0596
Real-Time Resting-state fMRI for Presurgical Mapping in Patients with Brain Tumors1Neurology, Physics and Astronomy, University of New Mexico, Albuquerque, NM, United States, 2Neurosurgery, University of New Mexico, Albuquerque, NM, United States, 3Neurology, University of New Mexico, Albuquerque, NM, United States
Synopsis
We investigated the feasibility of presurgical mapping in patients with brain tumors using real-time rsfMRI analysis methodology in combination with high-speed multi-band EPI. The objective was to map sensorimotor and language resting state networks in the vicinity of brain tumors and to monitor data quality online. We validated this approach in comparison with tfMRI and intra-operative electrocorticography (ECog). The data in patients show a high degree of consistency between resting state connectivity, task-based activation and ECS localization of motor cortex and Broca’s area. Localization of Wernicke’s area was more variable, both in rsfMRI and tfMRI.
Introduction
Preoperative task-based functional MRI (fMRI) is increasingly included in neurosurgery to aid the decision-making process of treatment of patients with brain lesions1-7. However, dependence on patient’s task-compliance, which may be impaired due to disability, is a limitation for clinical applications of task-based fMRI (tfMRI). Resting state functional MRI (rsfMRI) is a promising task-free approach to delineate eloquent cortex8-14, which may complement and potentially replace tfMRI in patient who are unable to perform required tasks15,16. However, rsfMRI is highly sensitive to head movement, physiological noise and spatial-temporal non-stationarity of resting state networks (RSNs)17,18. Online monitoring of data quality is desirable to ensure scan success19. In this study, we investigated the feasibility of presurgical mapping in patients with brain tumors using our recently developed real-time rsfMRI analysis methodology20 in combination with high-speed multi-band EPI, which is increasingly used for rsfMRI due to its high sensitivity resulting from unaliased sampling of physiological signal pulsation. The objective was to map sensorimotor and language resting-state networks in the vicinity of brain tumors and to monitor data quality in real-time. We validated this approach in comparison with tfMRI and intra-operative electrocorticography (ECog).Methods
RsfMRI (eyes open, 10min) and tfMRI (3min per task) data were acquired in 6 healthy controls (4F,2M) and in 3 patients (2F,1M) with brain tumors (1 glioblastoma, 2 low grade gliomas) using a 3T scanner equipped with 32-channel head coil. Informed written consent was obtained. Tasks were tailored to tumor location: motor (finger-tapping/fist-clenching), visual (eyes open/close), auditory (listening to syllables), and language (word/verb generation). MB8-EPI (TR/TE: 400/35ms, flip angle: 42o, voxel size: 3mm3, 32slices) was reconstructed and analyzed in real-time. Real-time seed-based connectivity analysis (SCA) of 2 RSNs and task-based correlation analysis were performed using the TurboFIRE tool20,21. Preprocessing included motion correction, 5mm isotropic Gaussian spatial filter, and spatial normalization into MNI space. SCA was performed with 8s moving average temporal low pass filter, 15s sliding window correlation analysis with running mean, and regression of 8 signal time courses from 6 rigid body motion parameters and WM and CSF ROIs. Motion parameters, true/false positive connectivity, and task-activation were monitored online. RSNs were mapped using unilateral Brodmann area (BA) based seed regions (auditory: AUN–BA41,42; default-mode: DMN–BA7,31; sensorimotor: SMN–BA01-03, visual: VSN–BA17, language: LAN-BA44,45 (Broca’s) and LAN-BA22,39,40 (Wernicke’s). Image guidance (Stealth Station Treon; Medtronic Surgical Navigation Technologies, Dublin, Ireland) for the surgical approach was based on clinical task-based presurgical fMRI obtained separately. Intraoperative brain mapping was performed using electro-cortical stimulation (ECS) and continuous electrocorticography (ECog). ECS locations were mapped onto stereotactic MRI and coordinates were recorded.Results
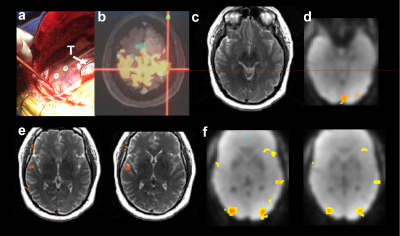
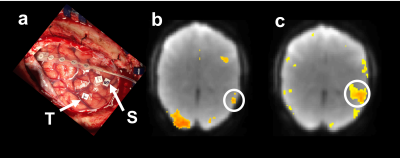
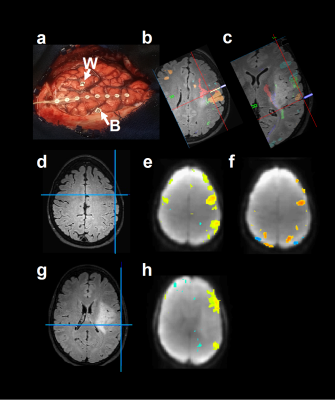
Online data quality monitoring enabled rapid optimization of scan protocols, early identification of task non-compliance and head-movement related false-positive connectivity prompting scan-repetition. Motor, sensory, and language networks in healthy controls were identifiable within 1min of scan time, stabilized within 5-10min and did not significantly change at 20min. Resting-state connectivity and task-based activation in the motor cortex in a patient with glioblastoma were localized within 5mm of the intra-operative ECS localization of the motor cortex (Figure 1). Resting-state language connectivity and task-based activation in Broca’s area in this patient were localized within ~10mm. Resting-state language connectivity and task-based activation in Wernicke’s area in a patient with low grade glioma were localized within 5mm of intra-operative ECS of speech arrest (Figure 2). Resting-state language connectivity and task-based activation in Broca’s area in a second patient with low grade glioma were localized within 5mm of intra-operative ECS of speech arrest (Figure 3). Resting-state connectivity in Wernicke’s area in this patient was more than 30mm posterior to the ECS based localization and 17mm posterior to (clinical) task-based fMRI. Resting-state connectivity and task-based activation in motor cortex in this patient were co-localized within 3mm.Discussion and Conclusions
The data in patients show a high degree of consistency between resting state connectivity, task-based activation and ECS localization of motor cortex and Broca’s area. Localization of Wernicke’s area was more variable, both in rsfMRI and tfMRI, and in the third patient discordant with intra-operative ECS localization, which may in part reflect cortical reorganization. Limitations of this study include small number of patients studied, atlas-based seed selection, which needs to be adapted to possible cortical reorganization due to neuroplasticity, and large spatial extent of sensorimotor and language connectivity in Broca’s area along the inferior-superior direction. Future work will include: iterative subject-specific seed optimization and intra-RSN functional parcellation combining rfMRI and tfMRI.Acknowledgements
Research reported in this publication was supported by NIH grant numbers 1R41NS090691 and R21EB018494. We thank Kimball Malherbe (Medtronics), Alam Syed, Troy Hutchins, and Abraham Dominguez for their support of data acquisition and analysis. Special thanks to Arvind Caprihan, Catherine Smith, and Diana South of Mind Research Network for their expert support in scanner operations.References
[1] S. Bookheimer, "Pre-surgical language mapping with functional magnetic resonance imaging," Neuropsychol Rev, vol. 17, pp. 145-155, Jun 2007.
[2] D. J. Lee, N. Pouratian, S. Y. Bookheimer, and N. A. Martin, "Factors predicting language lateralization in patients with perisylvian vascular malformations. Clinical article," J Neurosurg, vol. 113, pp. 723-730, Oct 2010.
[3] A. Tieleman, K. Deblaere, D. Van Roost, O. Van Damme, and E. Achten, "Preoperative fMRI in tumour surgery," Eur Radiol, vol. 19, pp. 2523-2534, Oct 2009.
[4] C. Stippich, "[Presurgical functional magnetic resonance imaging]," Radiologe, vol. 50, pp. 110-122, Feb 2010.
[5] A. Bizzi, V. Blasi, A. Falini, P. Ferroli, M. Cadioli, U. Danesi, D. Aquino, C. Marras, D. Caldiroli, and G. Broggi, "Presurgical functional MR imaging of language and motor functions: validation with intraoperative electrocortical mapping," Radiology, vol. 248, pp. 579-589, Aug 2008.
[6] J. J. Pillai and D. Zaca, "Relative utility for hemispheric lateralization of different clinical fMRI activation tasks within a comprehensive language paradigm battery in brain tumor patients as assessed by both threshold-dependent and threshold-independent analysis methods," Neuroimage, vol. 54 Suppl 1, pp. S136-145, Jan 2011.
[7] C. Giussani, F. E. Roux, J. Ojemann, E. P. Sganzerla, D. Pirillo, and C. Papagno, "Is preoperative functional magnetic resonance imaging reliable for language areas mapping in brain tumor surgery? Review of language functional magnetic resonance imaging and direct cortical stimulation correlation studies," Neurosurgery, vol. 66, pp. 113-120, Jan 2010.
[8] R. Li, K. Chen, A. S. Fleisher, E. M. Reiman, L. Yao, and X. Wu, "Large-scale directional connections among multi resting-state neural networks in human brain: a functional MRI and Bayesian network modeling study," Neuroimage, vol. 56, pp. 1035-1042, Jun 1 2011, 3319766.
[9] M. De Luca, C. F. Beckmann, N. De Stefano, P. M. Matthews, and S. M. Smith, "fMRI resting state networks define distinct modes of long-distance interactions in the human brain," Neuroimage, vol. 29, pp. 1359-1367, Feb 15 2006.
[10] M. D. Fox, A. Z. Snyder, J. L. Vincent, M. Corbetta, D. C. Van Essen, and M. E. Raichle, "The human brain is intrinsically organized into dynamic, anticorrelated functional networks," Proc Natl Acad Sci U S A, vol. 102, pp. 9673-9678, Jul 5 2005, 1157105.
[11] M. E. Raichle and A. Z. Snyder, "A default mode of brain function: a brief history of an evolving idea," Neuroimage, vol. 37, pp. 1083-1090; discussion 1097-1089, Oct 1 2007.
[12] V. Schopf, C. Windischberger, C. H. Kasess, R. Lanzenberger, and E. Moser, "Group ICA of resting-state data: a comparison," MAGMA, vol. 23, pp. 317-325, Dec 2010.
[13] A. Abou-Elseoud, T. Starck, J. Remes, J. Nikkinen, O. Tervonen, and V. Kiviniemi, "The effect of model order selection in group PICA," Hum Brain Mapp, vol. 31, pp. 1207-1216, Aug 2010.
[14] E. A. Allen, E. B. Erhardt, E. Damaraju, W. Gruner, J. M. Segall, R. F. Silva, M. Havlicek, S. Rachakonda, J. Fries, R. Kalyanam, A. M. Michael, A. Caprihan, J. A. Turner, T. Eichele, S. Adelsheim, A. D. Bryan, J. Bustillo, V. P. Clark, S. W. Feldstein Ewing, F. Filbey, C. C. Ford, K. Hutchison, R. E. Jung, K. A. Kiehl, P. Kodituwakku, Y. M. Komesu, A. R. Mayer, G. D. Pearlson, J. P. Phillips, J. R. Sadek, M. Stevens, U. Teuscher, R. J. Thoma, and V. D. Calhoun, "A baseline for the multivariate comparison of resting-state networks," Front Syst Neurosci, vol. 5, p. 2, 2011, 3051178.
[15] T. J. Mitchell, C. D. Hacker, J. D. Breshears, N. P. Szrama, M. Sharma, D. T. Bundy, M. Pahwa, M. Corbetta, A. Z. Snyder, J. S. Shimony, and E. C. Leuthardt, "A novel data-driven approach to preoperative mapping of functional cortex using resting-state functional magnetic resonance imaging," Neurosurgery, vol. 73, pp. 969-982; discussion 982-963, Dec 2013, PMC3871406.
[16] E. C. Leuthardt, M. Allen, M. Kamran, A. H. Hawasli, A. Z. Snyder, C. D. Hacker, T. J. Mitchell, and J. S. Shimony, "Resting-State Blood Oxygen Level-Dependent Functional MRI: A Paradigm Shift in Preoperative Brain Mapping," Stereotact Funct Neurosurg, vol. 93, pp. 427-439, 2015.
[17] K. R. Van Dijk, M. R. Sabuncu, and R. L. Buckner, "The influence of head motion on intrinsic functional connectivity MRI," Neuroimage, vol. 59, pp. 431-438, Jan 2 2012.
[18] T. D. Satterthwaite, D. H. Wolf, J. Loughead, K. Ruparel, M. A. Elliott, H. Hakonarson, R. C. Gur, and R. E. Gur, "Impact of in-scanner head motion on multiple measures of functional connectivity: Relevance for studies of neurodevelopment in youth," Neuroimage, vol. 60, pp. 623-632, 2012.
[19] N. U. F. Dosenbach, J. M. Koller, E. A. Earl, O. Miranda-Dominguez, R. L. Klein, A. N. Van, A. Z. Snyder, B. J. Nagel, J. T. Nigg, A. L. Nguyen, V. Wesevich, D. J. Greene, and D. A. Fair, "Real-time motion analytics during brain MRI improve data quality and reduce costs," Neuroimage, vol. 161, pp. 80-93, Aug 10 2017.
[20] S. Posse, E. Ackley, R. Mutihac, T. Zhang, R. Hummatov, M. Akhtari, M. Chohan, B. Fisch, and H. Yonas, "High-speed real-time resting-state FMRI using multi-slab echo-volumar imaging," Front Hum Neurosci, vol. 7, p. 479, 2013, 3752525.
[21] S. Posse, F. Binkofski, F. Schneider, D. Gembris, W. Frings, U. Habel, J. B. Salloum, K. Mathiak, S. Wiese, V. Kiselev, T. Graf, B. Elghahwagi, M. L. Grosse-Ruyken, and T. Eickermann, "A new approach to measure single-event related brain activity using real-time fMRI: Feasibility of sensory, motor, and higher cognitive tasks," Human Brain Mapping, vol. 12, pp. 25-41, Jan 2001.
Figures