0564
Cardiac MRI measured left atrial function can identify patient with pulmonary hypertension due to left heart disease.1Academic Radiology, The University of Sheffield, Sheffield, United Kingdom, 2Radiology, Sheffield Teaching Hospitals, Sheffield, United Kingdom, 3Sheffield Pulmonary Vascular Disease Unit, Sheffield Teaching Hospitals, Sheffield, United Kingdom
Synopsis
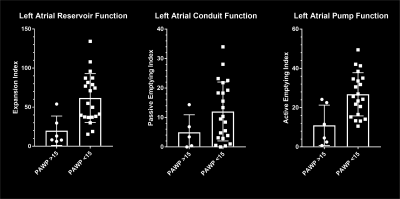
Patients with left heart disease commonly develop pulmonary hypertension (PH) [1], initially due to passive backward transmission of high left ventricular filling pressures through the pulmonary circulation. Assessment of left atrial reservoir and pump function using changes in left atrial area over time are useful to differentiate patients with left heart disease from other cases of suspected pulmonary hypertension (Mann-Whitney u test p-value 0.0015 and 0.0067 respectively).
INTRODUCTION
Patients with left heart disease commonly develop pulmonary hypertension (PH) [1], initially due to passive backward transmission of high left ventricular filling pressures through the pulmonary circulation. Previous non-invasive techniques using MRI measured left atrial volume index have been employed to identify patients with pulmonary hypertension due to left heart disease [2], however, this is a static representation of function and there are a number of patients mis-classified using left atrial volume index alone. The aim of this body of work was to assess functional metrics of the left atrium in the identification of patients with PH due to left heart disease.METHODS
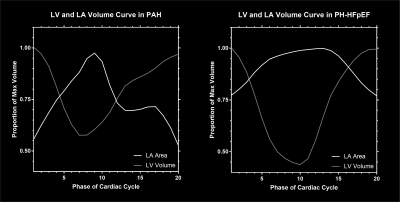
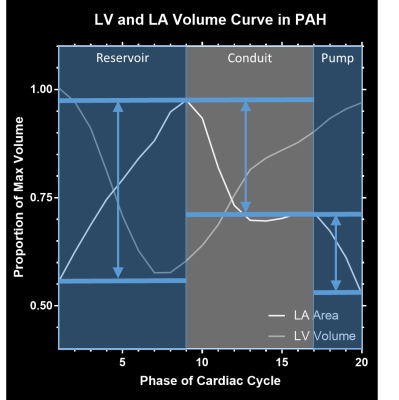
Patients with suspected pulmonary hypertension were prospectively consented for a cardiac MRI on a 1.5T GE HDx (GE Healthcare, Milwaukee, Wisconsin) using an 8 channel cardiac array coil. The left atrial function was analysed from LVLA (left ventricle-left atrial) steady state free procession images (SSFP) cardiac cine MRI. A single slice was acquired with the plane through the left atrium and left ventricle, retrospectively gated to the ECG with 20 phases. Sequence parameters were: slice thickness 8mm, TR 3.6ms, TE 1.5ms, acquisition matrix 256x256, field of view 512x512, flip angle 60˚, 125kHz bandwidth. Left atrial area was measured on each phase using Medis Q mass (Medis medical imaging systems, Leiden).The resultant left atrial area-time curve (see figure 1) was then analysed to assess for the reservoir, conduit and pump function. Figure 2 shows how each of the metrics of reservoir (expansion index), conduit (active emptying index) and pump (active emptying index) function were calculated using methods adapted from echocardiographic practise.RESULTS
44 patients with suspected PH were prospectively consented. 32 had right heart catheter also performed, and 29 had a measurable pulmonary arterial wedge pressure (PAWP). 2 cases had non-diagnostic images as the left atrium was not fully included in the image. 6 cases had PAWP >15mmHg and the remaining 21 cases had a normal PAWP.There was a significant difference in reservoir (expansion index) and pump (active emptying index) function between the cases with normal and raised PAWP (Mann-Whitney u test p-value 0.0015 and 0.0067 respectively). There was no significant difference in conduit function between the two groups (Mann-Whitney u test p-value 0.1319).CONCLUSIONS
There is a significant difference in left atrial reservoir and pump function between the patients with raised and normal pulmonary arterial wedge pressures, measured on MRI. This easy to measure metric may help to improve the identification of pulmonary hypertension due to left heart disease.Acknowledgements
This work was supported by NIHR grant NIHR-RP-R3-12-027, Wellcome grant 205188/Z/16/Z and MRC grant MR/M008894/1. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.References
[1] Guazzi M, Naeije R. Pulmonary Hypertension in Heart Failure. J. Am. Coll. Cardiol. 2017;69:1718–1734.
[2] Crawley SF, Johnson MK, Dargie HJ, et al. LA volume by CMR distinguishes idiopathic from pulmonary hypertension due to Hfpef. JACC Cardiovasc. Imaging. 2013;6:1120–1121.
Figures