0520
Can Negligible Hepatic Steatosis Determined by MRI-Proton Density Fat Fraction Obviate the Need for Liver Biopsy in Potential Liver Donors?1UHN, Toronto, ON, Canada
Synopsis
Hepatic steatosis in potential liver donor candidates has important implications towards outcomes of liver transplant recipients and donor safety. Hepatic steatosis in potential donors in excess of established but varying institutional thresholds are considered as grounds for donor ineligibility. However, negiblible/absent hepatic steatosis (<5%) is considered acceptable universally. Currently Liver biopsy is regarded as reference standard. We show in our study that MR-PDFF has very high NPV for excluding significant hepatic steatosis (>10%). Thus MRI-PDFF can be utilized for liver donor screening and obviates the need for liver biopsy when MRI-PDFF values are <5%
Introduction:
Living donor liver transplantation is crucial to the management of end-stage liver disease given the shortage of cadaveric liver graft availability. Prevalence rates of hepatic steatosis of 10-25 % have been described among living donors which has important implications for recipient and donor outcomes. There is high variability between institutional threshold for donor ineligibility based on the degree of hepatic steatosis with our center utilizing a threshold of 10%. However, the absence or negligible levels of hepatic steatosis (<5%) are considered universally acceptable for liver donation. At this time, liver biopsy is regarded as the reference standard for the assessment of donor hepatic steatosis.Purpose:
To determine whether magnetic resonance proton density fat fraction (MR-PDFF) of negligible hepatic fat percentage (<5%) can exclude significant hepatic steatosis (≥10%) in living liver donor candidates obviating the need for liver biopsy. To perform intra-individual comparisons between MR-PDFF techniques for hepatic steatosis quantification.Methods:
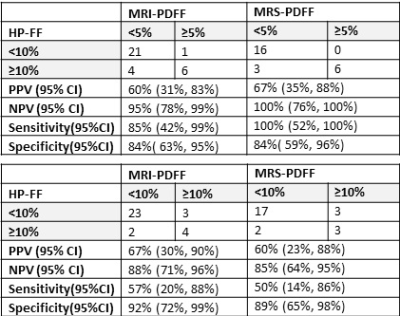
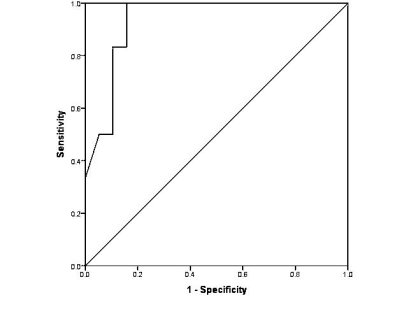
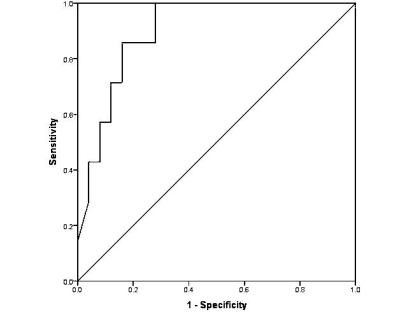
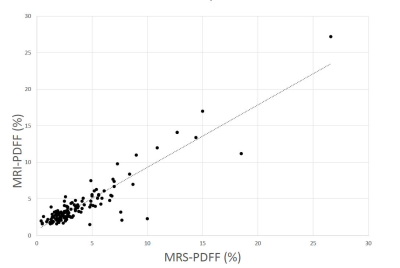
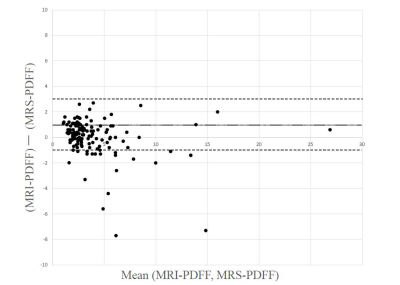
In an ethics board approved retrospective study, 144 consecutive liver donor candidates who had undergone Liver MRI with MR spectroscopy (MRS) and Multi-echo Dixon (6ED) were included. Both 1.5T and 3.0T systems (Siemens Avanto fit and Verio fit, Siemens Healthcare, Erlangen, Germany) were used. MRS was performed using a T2-corrected multi-echo 1H spectroscopy sequence (HISTO). This involves a series of five single-voxel STEAM sequences concatenated with a fixed TR of 3000 ms with acquired TE’s of 12, 24, 36, 48 and 72 ms. Using 3 plane-localizing images, single 3 × 3 × 3 cm voxel was placed in the liver avoiding vascular and biliary structures with liver margins being at least 2 cm away from the voxel boundary. Multi-echo Dixon sequence used six fractional echoes (TE=1.05, 2.46, 3.69, 4.92, 6.15 and 7.38 ms) in a single breath hold. Fat fraction (MRI-PDFF) was quantified by placing a large (≥2.0 cm2) elliptic region of interest (ROI) on the MRI fat fraction map in a homogeneous region of liver with care to avoid vascular and biliary structures.MR Spectroscopy fat fraction (MRS-PDFF) was recorded from the in line report generated by the HISTO sequence. A subset of 32 candidates underwent liver biopsy. An experienced pathologist quantified degree of steatosis in increments of 5% starting from 0% and this was designated as the histopathology determined fat fraction in our analysis (HP-FF). Hepatic fat percentage was determined using MR-PDFF with histopathology (HP-FF) as reference standard.ROC analysis with PPV, NPV, sensitivity and specificity was performed to discriminate between clinically significant steatosis (≥10%) or not (<10%) at MRS-PDFF and MRI-PDFF thresholds of 5% and 10%. Pearson correlation and Bland-Altman analysis between MRS-PDFF and MRI-PDFF was performed for intra-individual comparison of hepatic steatosis estimationResults:
HP-FF values ranged from 0 to 40% with a mean of 6 ± 9%. Values for MRI-PDFF ranged from 2% to 15% with a mean of 6 ± 4% while MRS-PDFF ranged from 1% to 52% with a mean of 7 ± 11 %. There was significant association between MRS-PDFF and MRI-PDFF with HP-FP. High NPV of 95% (95% CI: 78%, 99%) and 100% (95% CI: 76%, 100%) as well as AUC of 0.90 (95% CI: 0.79, 1.0) and 0.93 (95% CI: 0.84, 1.0) were obtained with cut-off threshold of 5% MRI-PDFF and MRS-PDFF respectively to exclude clinically significant steatosis (≥10%). (Fig.1-3). Intra-individual comparison between MRS-PDFF and MRI-PDFF showed a Pearson correlation coefficient of 0.83. (Fig.3) Bland-Altman analysis showed a mean difference of 1% with 95% limits of agreement between -1% and 3%(Fig. 5)Discussion:
Using histopathology as a reference standard, we established the ability of MRS and MRI to distinguish between donors without and with significant (≥ 10%) hepatic steatosis. Specifically, we were able to establish very high to perfect negative predictive values for MRI (95%) and MRS (100%) to exclude the presence of hepatic steatosis equal to or greater than 10% which is considered beyond a safe margin for transplantation at our institution. Our institutional threshold of 10% would be considered more conservative as thresholds as high as 20% or 30% have been reported at some centers over concerns of over-restricting the liver donor pool. The robust performance of MRS and MRI in our study for the relatively conservative threshold of 10% would only be expected to improve at institutions where higher levels of hepatic steatosis are considered acceptable.We also noted a low mean difference between MRS-PDFF and MRI-PDFF of 1% with Bland-Altman analysis.Conclusion:
MR-PDFF estimate of negligible hepatic fat percentage (<5%) has sufficient NPV for excluding clinically significant hepatic steatosis (≥ 10%) in living liver donor candidates obviating the need for liver biopsy. It maybe sufficient to acquire only the multi-echo Dixon MRI-PDFF for hepatic steatosis estimationAcknowledgements
NoneReferences
1. Lee JY, Kim KM, Lee SG, Yu E, Lim YS, Lee HC, et al. Prevalence and risk factors of non-alcoholic fatty liver disease in potential living liver donors in Korea: a review of 589 consecutive liver biopsies in a single center. J Hepatol 2007;47(2):239-244.
2. Perez-Daga JA, Santoyo J, Suárez MA, Fernández-Aguilar JA, Ramírez C, Rodríguez-Cañete A, et al. Influence of degree of hepatic steatosis on graft function and postoperative complications of liver transplantation. Transplant Proc 2006;38: 2468-2470.
3. Nagai S, Fujimoto Y, Kamei H, Nakamura T, Kiuchi T. Mild hepatic macrovesicular steatosis may be a risk factor for hyperbilirubinaemia in living liver donors following right hepatectomy. Br J Surg 2009; 96(4):437-444.
4. Kim SH, Lee JM, Han JK, Lee JY, Lee KH, Han CJ, et al. Hepatic macrosteatosis: predicting appropriateness of liver donation by using MR imaging—correlation with histopathologic findings. Radiology 2006;240(1):116-129.
5. Ryan CK, Johnson LA, Germin BI, Marcos A. One hundred consecutive hepatic biopsies in the workup of living donors for right lobe liver transplantation. Liver Transpl 2002;8(12):1114-1122.
6. Reeder SB, Cruite I, Hamilton G, Sirlin CB. Quantitative assessment of liver fat with magnetic resonance imaging and spectroscopy. J Magn Reson Imaging 2011;34(4):729-749.
7. Bohte AE, van Werven JR, Bipat S, Stoker J (2011) The diagnostic accuracy of US, CT, MRI and 1H-MRS for the evaluation of hepatic steatosis compared with liver biopsy: a meta-analysis. Eur Radiol 2011;21:87-97.
8. Satkunasingham J, Besa C, Bane O, Shah A, de Oliveira A, Gilson WD et al. Liver fat quantification: Comparison of dual-echo and triple-echo chemical shift MRI to MR spectroscopy. Eur J Radiol. 2015;84(8):1452-8.
9. Yoon JH, Lee JM, Suh KS, Lee KW, Yi NJ, Lee KB, et al. Combined use of MR fat quantification and MR elastography in living liver donors: can it reduce the need for preoperative liver biopsy? Radiology 2015;276(2):453-464.
Figures