0492
Identification of high-risk plaque features in intracranial atherosclerosis: initial experience using high-resolution MRI with a quantitative radiomics approach1Radiology, Changhai Hospital, Shanghai, China, 2Radiology, University of California, San Francisco, CA, United States
Synopsis
This study aims to evaluate a radiomic approach including texture analysis based on HR-MRI to differentiate acute symptomatic plaque from asymptomatic plaque. 94 patients with basilar artery stenosis underwent HR-MRI. The stenosis value, plaque area/burden, lumen area, intraplaque hemorrhage (IPH), contrast enhancement ratio and 94 quantitative radiomic features were extracted. Multivariate logistic analysis and a random forest model were performed. Results: IPH and enhancement ratio were independently associated with acute symptoms. Radiomic features in T1 and CE-T1 images were associated with acute symptoms. The combined T1 and CE-T1 radiomic approach had a significantly higher AUC of 0.940. Conclusion: Radiomic analysis accurately distinguished between acutely symptomatic plaques and asymptomatic plaques.
Introduction
Intracranial atherosclerotic disease (ICAD)is associated with frequent stroke recurrence, and high resolution vessel wall magnetic resonance imaging (HR-MRI) can provide atheroma information related to its vulnerability and activity. Although many studies have shown differences in radiological features between intracranial atherosclerotic plaques with and without activity, they lacked quantitative features, which could be utilized as predictors of genetics and clinical outcomes. This study aims to evaluate a quantitative radiomic approach including texture analysis based on HR-MRI to differentiate acute symptomatic basilar artery plaque from chronic/asymptomatic plaque.Methods
Study population: 94 patients with basilar artery stenosis underwent HR-MRI between January 2014 and December 2015. Patients were scanned with T1 and T2 weighted imaging, and T1 imaging following Gd contrast injection (CE-T1).
Imaging analysis: All images were analyzed by four radiologists. Each detected plaque was independently classified as acute/sub-acute/chronic symptomatic if a lesion was shown on conventional neuroimaging (T2 FLAIR and DWI showed infarct) after an acute (<4 weeks), sub-acute (4-12 weeks) or chronic (>12 weeks) ischemic stroke/TIA with accompanying clinical symptoms. The stenosis value, plaque area/burden, lumen area, intraplaque hemorrhage (IPH), contrast enhancement ratio and 94 quantitative radiomic features were extracted and compared between acute/sub-acute and chronic/asymptomatic patients using CMR Tools software (Cardiovascular Imaging Solutions Ltd, UK). The radiomic features were analyzed by two reviewers who independently measured the radiomic features in a subset of patients (n=40) which were randomly selected from the study population. Each reviewer segmented the plaque boundaries at the level of the largest plaque area on T1, T2 and CE-T1 images. For each sequence, 94 radiomic features including intensity (maximal intensity, mean intensity, standard deviation of intensity, etc), shape based feature (area, length, etc), and textures were extracted and analyzed according to a previous publication. [1]
Statistical analysis: Univariate analysis was first performed to assess the association between each variable and acute symptomatic status. Multivariate analysis was performed which included the variables that had p<0.05 in the univariate tests. The odds ratios (OR) with 95 % confidence intervals (CI) was calculated by a logistic regression model with stepwise selection of variables. T-tests were used to first select the features with p<0.05 in each sequence, and these features were set as input for the random forest training features.[2]
Results
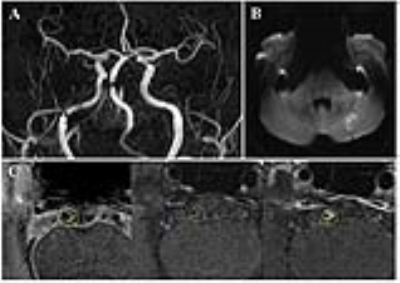
A total of 139 patients met the
inclusion criteria. 45 patients were excluded due to intracranial aneurysm
(n=31), moyamoya disease (n=5), vasculitis (n=4), dissection (n=3) and bad
image quality (n=2). As a result, 94 patients were included in the final
analysis. Sample patient images are
shown in Figure 1 and 2. The demographic data of the patients is shown in Figure
3. IPH and enhancement ratio were independently
associated with acute symptoms (odds ratio [OR] =
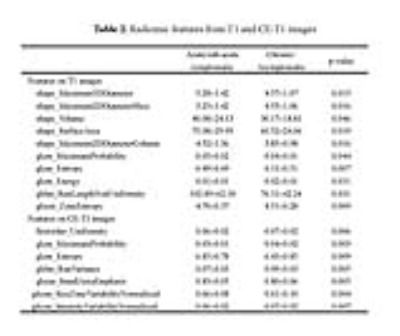
6.541, 95% CI, 1.396-30.644 and OR=9.028, 95% CI, 1.045-78.023, respectively). Radiomic features
in T1 and CE-T1 images were associated with acute symptoms, but the features in
T2 images were not. (Figure 4) The combined IPH
and enhancement ratio had an area under the curve (AUC) of 0.700 for
identifying acute/sub-acute symptomatic plaques, and the combined T1 and CE-T1
radiomic approach had a significantly higher AUC of 0.940. Combination of all
features reached an AUC of 0.950, with sensitivity of 87.5% and specificity of 91.8%, and accuracy of 86.2%. (Figure 5)Discussion
To our knowledge, this study similarly extends
radiomic analysis of intracranial plaque by classifying intracranial basilar
artery plaque into acute/sub-acute symptomatic versus chronic/asymptomatic
based on quantitative information extracted from HR-MRI. Radiomic analysis has
the benefit of identifying quantitative variables within imaging data to
improve accuracy (86.2% as shown in this study) and diagnostic confidence
beyond conventional measurements. The favorable accuracy values in this study
over those previously reported by conventional HR-MRI support the use of
radiomic analysis to improve identification of acute symptomatic plaque. It is
hoped that radiomic approaches applied to HR-MRI of the basilar artery will
result in improved accuracy of stroke risk assessment, which is especially
important given the high-risk nature of symptomatic basilar artery ICAD. This
risk assessment could then be used to initiate more effective secondary
prevention strategies by more appropriately assigning high-risk patients with
posterior circulation ischemic events due to non-stenotic plaque to more
aggressive dual antiplatelet therapy.
Conclusion
Radiomic analysis of basilar artery plaque texture on HR-MRI accurately distinguished between plaques in patients who were acutely symptomatic and plaques in patients who were chronic/asymptomatic. The highest accuracy was achieved by combining radiomic features with assessment of intraplaque hemorrhage and plaque enhancement.Acknowledgements
No acknowledgement found.References
[1] Aerts HJ, Velazquez ER, Leijenaar RT, et al. Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nat Commun. 2014;5:4006 [2] Shi T, Seligson D, Belldegrun AS, et al. Tumor classification by tissue microarray profiling: Random forest clustering applied to renal cell carcinoma. Mod Pathol. 2005;18:547-557Figures