0487
Vascular risk factors and intracranial atherosclerosis at 7T vessel wall MRI in Caucasian ischemic stroke and TIA patients1Radiology, UMC Utrecht, Utrecht, Netherlands, 2Neurology, UMC Utrecht, Utrecht, Netherlands, 3Epidemiology, UMC Utrecht, Utrecht, Netherlands
Synopsis
There is a lack of knowledge on the association between cardiovascular risk factors and intracranial atherosclerotic lesion burden in the Caucasian population. In this study 105 Caucasian stroke and TIA patients underwent 7T intracranial vessel wall imaging within 3 months after symptom onset. Poisson regression analysis showed that older age, higher systolic blood pressure, diabetes mellitus and a higher SMART risk score (wherein multiple cardiovascular risk factors are combined) were associated with a higher number of vessel wall lesions. Controversially, dyslipidemia and cigarette smoking were not associated with the severity of intracranial vessel wall lesions.
Introduction
Intracranial atherosclerosis (ICAS) is one of the most important causes of ischemic stroke1. Although general vascular risk factors have all been – variably – correlated to ICAS, current knowledge is mainly based on angiographic studies assessing atherosclerosis at an advanced stage resulting in calcifications or stenoses2. Also, these studies have mainly been performed in the Asian population. In light of the differences in prevalence and severity of intracranial atherosclerosis between racial groups, as well as previous publications showing that only approximately 25% of intracranial vessel wall lesions causes detectable stenosis3,4, we sought to determine the association between cardiovascular risk factors and intracranial atherosclerosis in a Caucasian population, using vessel wall MR imaging (VWI).Methods
In this single-center cross-sectional cohort study, between 2009 and 2017, 105 patients were included for 7T intracranial VWI within three months after an ischemic stroke or transient ischemic attack (TIA) of the anterior cerebral circulation. Until July 2011, a small field-of-view intracranial VWI sequence (magnetization-prepared inversion recovery turbo-spin-echo (MPIR-TSE) sequence5, 0.8x0.8x0.8mm3 spatial resolution), was used, on which only the anterior circulation arteries could be assessed; patients included after July 2011 underwent a (then-developed) whole-brain sequence (same spatial resolution)6 enabling assessment of anterior and posterior circulation. Number, location and enhancement of vessel wall lesions was scored on both pre- and postcontrast images. Baseline characteristics and vascular risk factors including the SMART risk score (includes multiple cardiovascular determinants and, therefore, may act as a multivariate analysis) were collected7. Poisson regression analysis was performed to investigate the association between the number of intracranial vessel wall lesions and vascular risk factors.Results
Ninety patients were suitable for analysis. Patient characteristics including known vascular risk factors are shown in Table 1. Age (p=0.005), systolic blood pressure (p=0.017), diabetes mellitus (p=0.001) and the SMART risk score (p=0.025) showed a significant correlation with the number of anterior vessel wall lesions (Figure 1). This correlation remained significant for age and diabetes mellitus after adjustment for sex and age (p=0.002 and p=0.009 respectively) (Table 2). For the total lesion burden (anterior and posterior lesions; n=45), age, systolic blood pressure and diabetes mellitus were significantly correlated and, including eGFR, also showed an significant correlation after adjustment for age and sex (p < 0.05 in all cases) (Table 3).Discussion
In this study performed in a Caucasian ischemic stroke and TIA population, age, systolic blood pressure, diabetes mellitus and the SMART risk score were significantly associated with the number of anterior intracranial vessel wall lesions, although after adjustment for age and sex only diabetes mellitus remained. For the total burden of vessel wall lesions (anterior and posterior), systolic blood pressure, diabetes mellitus and eGFR also remained significantly correlated after adjustment. Interestingly, the other vascular risk factors like dyslipidemia and smoking did not show any significant correlation with the number of vessel wall lesions.
Due to heterogeneity in study population, diagnostic methods and varying definition of ICAS of previously published studies, these results are difficult to compare with the current study. Overall, most studies have been performed in the Asian population using lumenographic methods. Advanced age, hypertension, diabetes mellitus, hyperlipidemia, glycosuria, and a (family) history of cardio- or cerebrovascular disease were previously identified as potential risk factors for ICAS1. Age, hypertension and diabetes are well established risk factors for ICAS2, which is reflected in the results from the current study held in the Caucasian population. Other studies also showed dyslipidemia and cigarette smoking as risk factors for ICAS2,3; however, this could not be reproduced in our study. Possible explanations may be that these risk factors are only associated with certain ethnic populations or with the more advanced stages of ICAS, in which luminal narrowing develops3. Alternatively, since there has still been no validation of any intracranial VWI sequence with histology, it may be that the vessel wall lesions that were scored in this study not only represent atherosclerotic plaques but also vessel wall thickness fluctuation due to ageing, thereby underestimating any correlation with these risk factors.
Conclusion
Older age, higher systolic blood pressure, diabetes mellitus and a higher SMART risk score were associated with a higher number of vessel wall lesions in a Caucasian population of stroke and TIA patients. Controversially, dyslipidemia and cigarette smoking were not associated with the severity of intracranial vessel wall lesions. Future studies should assess whether this is due to overcalling of vessel wall lesions on intracranial VWI sequences, or reflecting a less important role for these risk factors in the development of (early) atherosclerosis.Acknowledgements
No acknowledgement found.References
1. Gorelick P, Wong KS,
Liu L. Epidemiology. Frontiers of neurology and neuroscience 2016;40:34-46.
5. van der Kolk AG, Zwanenburg JJ,
Brundel M, et al. Intracranial vessel wall imaging at 7.0-T MRI. Stroke;
a journal of cerebral circulation 2011;42:2478-84.
6. van der Kolk AG,
Hendrikse J, Brundel M, Biessels GJ, Smit EJ, Visser F. Multi-sequence
whole-brain intracranial vessel wall imaging at 7.0 tesla. European radiology
2013;23:2996-3004.
7. Dorresteijn
JA, Visseren FL, Wassink AM, et al. Development and validation of a prediction rule for
recurrent vascular events based on a cohort study of patients with arterial
disease: the SMART risk score. Heart 2013;99:866-72.
Figures
Table 1. Patient characteristics of the 90
patients included for analysis. Body Mass Index was
measured as kilograms divided by height in meters squared.
Table
3. Crude and adjusted rate ratios (for age and sex) including their 95%
confidence intervals (CI) for the total number of lesions. A p-value <0.05
was considered statistically significant. LDL; Low Density Lipoprotein, HDL;
High Density Lipoprotein, eGFR; estimated Glomerular Filtration Rate, SMART;
Second manifestations of arterial disease, this estimates the 10-year risk for
recurrent vascular event in patients with manifest cardiovascular disease. Bold, statistically significant
correlations.
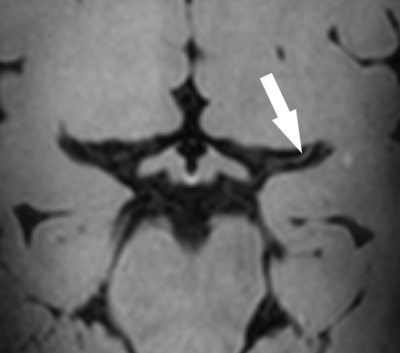
Figure 1. A 41-year old female with a recent left-sided stroke. Besides a positive family history of cardiovascular disease, no other cardiovascular risk factors were present. On postcontrast 7T T1-weighted MPIR-TSE (Magnetization-Prepared Inversion Recovery Turbo Spin Echo) vessel wall images an eccentric vessel wall thickening is seen in the left middle cerebral artery (white arrow).