0486
Increases in the Prevalence of Subclinical Cerebrovascular Atherosclerosis with Age: A 3.0 T Magnetic Resonance Imaging Study of Community-based AdultsXihai Zhao1, Gaifen Liu2, Runhua Zhang2, Xiaoyi Chen3, Dongye Li3, Yong Jiang2, Yilong Wang2, Yongjun Wang2, and Chun Yuan1,4
1Center for Biomedical Imaging Research, Department of Biomedical Engineering, Tsinghua University School of Medicine, Beijing, China, 2Department of Neurology, Beijing Tiantan Hospital, Beijing, China, 3Center for Brain Disorders Research, Capital Medical University and Beijing Institute for Brain Disorders, Beijing, China, 4Department of Radiology, University of Washington, Seattle, WA, United States
Synopsis
It is well established that atherosclerotic diseases occurring in intracranial and extracranial carotid arteries are associated with ischemic cerebrovascular events. It is important to find a surrogate risk factor for subclinical cerebrovascular atherosclerosis in asymptomatic subjects for stroke prevention. This study sought to investigate the association between age and subclinical cerebrovascular atherosclerosis in community-based adults using MR vessel wall imaging. We found that the prevalence of cerebrovascular atherosclerotic plaques increased with age. The association between age and cerebrovascular atherosclerosis suggests that age was an independent indicator for subclinical cerebrovascular atherosclerosis.
Introduction and Purpose
It is well established that atherosclerotic diseases occurring in intracranial and extracranial carotid arteries are associated with ischemic cerebrovascular events. Early identification of cerebrovascular atherosclerosis in asymptomatic individuals is important for stroke prevention. Magnetic resonance imaging vessel wall imaging, particularly three-dimensional imaging techniques, is the best non-invasive tool for plaque characterization. Apparently, MR imaging is not a cost-effective screening tool for atherosclerosis. Therefore, it is warranted to find a surrogate risk factor for cerebrovascular atherosclerosis in asymptomatic subjects. Previous studies have shown that age is associated with carotid and intracranial artery atherosclerosis [1-3]. However, the relationship between age and subclinical cerebrovascular plaques in Chinese community-based population is unknown. The purpose of this study is to investigate the association between age and subclinical cerebrovascular atherosclerosis in community-based adults using MR vessel wall imaging.Methods
Study sample: The subjects were recruited from a community study of CAMERA-TSINGHUA in which cerebrovascular disease risk was investigated in community-based population. All subjects underwent MR vessel wall imaging for both intracranial and extracranial carotid arteries. The study protocol was approved by institutional review board and written consent form was obtained by each subject. MR imaging: The T1-VISTA and 3D-MERGE imaging sequences were acquired for intracranial and extracranial carotid arteries respectively on a 3.0T MR scanner (Achieva TX, Philips Healthcare) with a custom-designed 36-channel neurovascular coil and the following parameters: T1-VISTA: turbo spin echo; repeat time (TR)/echo time (TE) 700/21 ms, flip angle 90°, field of view (FOV) 20x20x4.5 cm3, and spatial resolution 0.6x0.6x0.6 mm3; and 3D MERGE: fast field echo, TR/TE 9/4.2 ms, flip angle 6°, FOV 25x16x4 cm3, and spatial resolution 0.8x0.8x0.8 mm3. Image analysis: MR images were reviewed by two radiologists with >5 years’ experience in cardiovascular imaging using a custom-designed software with consensus. Presence/absence of atherosclerotic plaque which is defined as eccentric wall thickening in the vessel wall was determined in intracranial and extracranial carotid arteries. Statistical analysis: The subjects were divided into 6 groups by age: <40 years, 40-49 years, 50-59 years, 60-69 years, 70-79 years, and ≥ 80 years. Prevalence of atherosclerotic plaque in intracranial artery, extracranial carotid artery, and both intra- and extracranial carotid arteries was calculated in each age group. The relationship between age and presence of cerebrovascular plaque was assessed to calculate odds ratio (OR) and corresponding 95% confidence interval (CI) using logistic regression model.Results
Of 476 recruited asymptomatic subjects (mean age, 61.4±13.9 years; 195 males), 14 (2.9%), 206 (43.3%), and 57 (12%) had subclinical atherosclerotic plaque in intracranial artery only, extracranial carotid artery only, and both intracranial and extracranial carotid arteries, respectively. An increasing trend was found in the prevalence of plaques in each cerebrovascular bed with age (Fig. 1). Univariate logistic regression showed that age was significantly associated with presence of atherosclerotic plaque in intracranial artery only (OR=1.77, 95% CI 1.34-2.35, p<0.0001), extracranial carotid artery only (OR=1.42, 95% CI 1.31-1.55, p<0.0001), and both intracranial and extracranial arteries (OR=1.79, 95% CI 1.53-2.10, p<0.0001) with increment of 5 years. After adjusted for confounding factors of gender, body mass index, hypertension, smoke, diabetes, and levels of lipoproteins, above associations remained statistically significant (all p<0.001, Table 1). Fig. 2 represents example for an old subject with subclinical atherosclerotic plaques in both intracranial and extractranial carotid arteries.Discussion and Conclusion
In the present study, the prevalence of cerebrovascular atherosclerotic plaques was found to be increasing with age. The association between age and cerebrovascular atherosclerosis suggests that age was an independent indicator for subclinical cerebrovascular atherosclerosis. Previous studies have shown that the arterial compliance [4] and function of endothealial cells [5] will decline with age which may lead to arteries becoming more susceptible to developing atheroma. In addition, we found that 12.8% of subjects <40 years old had carotid plaque but none had intracranial artery plaques, indicating that atherosclerotic disease may initiate earlier in carotid arteries than that in intracranial arteries.Acknowledgements
This study is supported by grants of Beijing Municipal Science and Technology Commission (D131100002313002) and Beijing Municipal Commission of Health and Family Planning (2016-1-2041).References
- Fine-Edelstein JS, Wolf PA, O'Leary DH, et al. Precursors of extracranial carotid atherosclerosis in the Framingham Study. Neurology. 1994;44(6):1046-50.
- Qureshi AI, Caplan LR. Intracranial atherosclerosis. Lancet. 2014;383(9921):984-98.
- Ding X, Li C, Yu K, et al. Different risk factors between intracranial and extracranial atherosclerotic stenosis in Asian population: a systematic review and meta-analysis. Int J Neurosci. 2014;124(11):834-40.
- Lee HY, Oh BH. Aging and arterial stiffness. Circ J. 2010;74(11):2257-62.
- Minamino T, Miyauchi H, Yoshida T, et al. Endothelial cell senescence in human atherosclerosis: role of telomere in endothelial dysfunction. Circulation. 2002;105(13):1541-4.
Figures
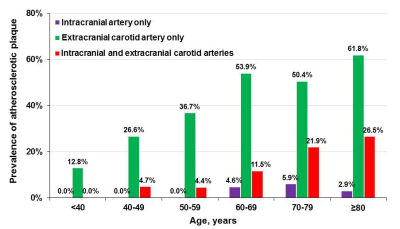
Figure 1. Prevalence of cerebrovascular atherosclerosis among different age group.
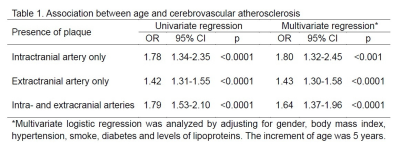
Table 1. Association between age and cerebrovascular atherosclerosis.
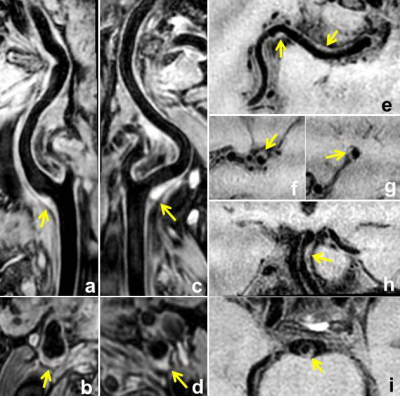
Figure 2. The MR images are from a 70 years old male subject. Multiple atherosclerotic plaques (yellow arrows) were found in bilateral carotid arteries (a-d), right middle cerebral artery (e-g), and basilar artery (h, i). b, d, f, g, and i are the corresponding axial images for right (a) and (c) left carotid atery, right middle cerebral artery (e), and basilar artery (h).