0377
Three Dimensional Intra- and Extra-cranial Arterial Vessel Wall Joint Imaging in Patients with ischemic strokeNa Zhang1, Lin Jia2, Jinhao Lyu3, Lei Zhang1, Wenxiao Jia2, Hairong Zheng1, and Xin Liu1
1Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, shenzhen, China, 2XinJiang Medical University, Urumchi, China, 3Department of Radiology, Chinese PLA General Hospital, Beijing, China
Synopsis
Intracranial and carotid atherosclerotic plaques are responsible for about 75% of ischemic stroke, the leading cause of mortality and morbidity worldwide. A 3D intra- and extra-cranial arterial vessel wall joint imaging was developed for simultaneously evaluating intracranial and carotid arterial plaques. The aim of this study was to assess the clinical potential of the 3D joint imaging technique in a large-scale patients with recent cerebrovascular symptoms. In general, this joint imaging method allows satisfactory image quality and comprehensive evaluation of atherosclerotic disease, and it has great potential to be used for optimizing treatment.
Introduction
Stroke remains a leading cause of mortality and morbidity worldwide, and ischemic stroke accounts for about 80% of the cases. The major underlying cause of ischemic stroke is atherosclerosis, and intracranial and carotid atherosclerotic plaques are responsible for about 75% of ischemic stroke. High resolution vessel wall magnetic resonance (MR) imaging can directly visualize the vessel wall and has demonstrated the potential to characterize plaque features which are intimately associated with recent clinical events [1-4]. Recently, a three dimensional (3D) intra- and extra-cranial arterial vessel wall joint imaging was developed at 3.0 T MR system based on T1-weighted 3D variable-flip-angle turbo spin-echo sequence (SPACE) combined with delay alternating with nutation for tailored excitation (DANTE) module [5]. This joint imaging method can simultaneously assess intracranial and carotid arterial plaques with improved cerebrospinal fluid and blood suppression, large spatial coverage and time-saving than current SPACE protocols which using multiple scans to cover all frequently affected vascular locations. However, a large-scale clinical evaluation of the technique has yet to be conducted, particularly in patients with cerebrovascular ischemic events. The aim of this study was to assess the clinical potential of the newly developed intra- and extra-cranial arterial vessel wall joint imaging technique in patients with intra- and/or extra-cranial atherosclerosis disease.Materials and Methods
This prospective study was approved by the local institutional review board. Written informed consent was obtained from all patients before MR imaging. From April 2016 through September 2017 in a single imaging center, 55 consecutive patients with clinically confirmed recent cerebrovascular symptoms (46 males, ages 13- 69, mean 45.53±12.06 years) were recruited to underwent 3D intra- and extra-cranial arterial vessel wall joint imaging with and without contrast enhancement on a 3T MR system (MAGNETOM TIM Trio, Siemens Medical Solution, Germany). Exclusion criteria included general contraindications to MR examination and a renal clearance of < 30 mL/min. A custom designed 32-channel head (24 channels) and neck (4 channels on each side) coil was used for signal reception. All subjects were placed head first and in a supine position. The foam padding was used to immobilize the head to prevent movement. Relevant imaging parameters were: spatial resolution = 0.55 × 0.55 × 0.55 mm3 without interpolation, sagittal orientation, GRAPPA 2, scan time 9 min 6 sec. Image quality based on a four point score, number of plaques and culprit plaque according to Qiao et al [6] were evaluated in consensus by two radiologists (L. J. and J. L.) with more than 6-year experience in vascular MR.Results
All patients successfully underwent MR scans with and without contrast agent. Characteristics of the 55 patients were detailed in Table 1. The image quality scores for intracranial internal carotid artery (ICA) and middle cerebral artery (MCA), basilar artery (BA) and vertebral artery (VA), and extracranial carotid artery (CA) were summarized in Table 2. There was no significant difference between pre and post contrast vessel wall MR images (p > 0.05). Except 3 dissection (Figure 1), 2 moyamoya, 2 vasculitis, and 5 who had no obvious cause or atherosclerotic plaque formation, 150 plaques were detected in 43 patients with multiple plaques found in 36 patients (84%) (range 1 to 8 plaques, mean 3.56 plaques per patient). Of which, 122 (81%) and 28 (19%) plaques were identified in intracranial and extracranial arteries, respectively. The culprit plaques were also identified for all 43 patients with atherosclerotic plauqes. 63 (100% enhanced) and 22 (79% enhanced) culprit plaques were identified in intracranial and extracranial arteries, respectively. A culprit plaque with its downstream infarction is shown in Figure 2.Discussion and Conclusion
In general, the intra- and extra-cranial arterial vessel wall joint imaging allows satisfactory image quality for the delineation of vessel wall and provides large spatial coverage of common sites of atherosclerosis formation. The combined 3D imaging technique allows comprehensive evaluation of atherosclerotic disease in intra and extracranial arteries. This combined 3D MR imaging method has the ability to classify ischemic stroke etiology subtype and identify culprit plaques for both intra- and extracranial arteries. In conclusion, this joint imaging is a promising vessel wall MR imaging method for comprehensive diagnosis of cerebrovascular symptoms and investigation of etiology, and has great potential to be used for optimizing treatment.Acknowledgements
This work was supported in part by National Key R&D Program of China (2016YFC0100100), and Key Laboratory for Magnetic Resonance and Multimodality Imaging of Guangdong Province (2014B030301013).References
[1] Fan Z et al. MRM 2017; 77(3):1142-1150. [2] Qiao Y et al. JMRI 2011; 34:22-30. [3] van der Kolk AG et al. Eur Radiol. 2013; 23:2996-3004. [4] Zhang N et al. MRI 2017; 39:89-97. [5] Zhang L et al. MRI 2017; 44:65-71. [6] Qiao Y et al. Radiology 2014; 271(2):534-542.Figures
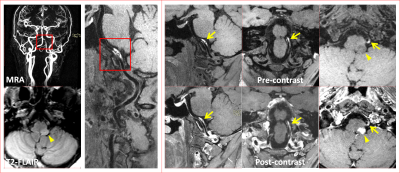
Figure 1 Representative 3D
intra- and extra-cranial vessel wall joint images with (post-contrast) and
without (pre-constrast) contrast agent in a 47-year-old female patient with
sub-acute ischemic stroke. Contrast enhanced magnetic resonance angiography
(MRA) shows stenosis of left vertebral artery. 3D pre- and post-contrast vessel
wall images show the dissection at the corresponding
location (arrows) with high signal intensity in both pre- and post-contrast
images. The downstream infarct lesion is observed in left medulla oblongata (arrowhead).
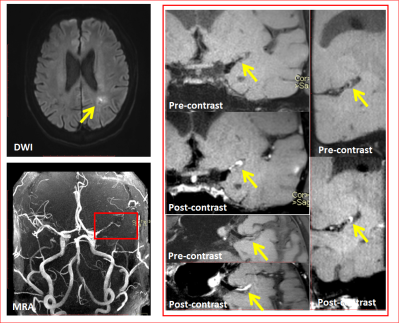
Figure 2 Representative MR images
of a 39-year-old male patient with a single acute infarct lesion. TOF MRA shows
stenosis of left middle cerebral artery. An eccentric atherosclerotic plaque detected
at the corresponding location (arrows) on 3D vessel wall images is considered as the culprit lesion with obvious enhancement similar to
pituitary on post-contrast images.
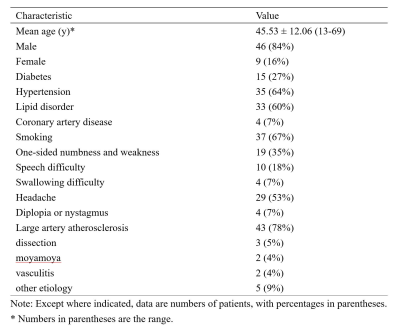
Table 1 Characteristics of
the 55 patients with recent cerebrovascular symptoms.
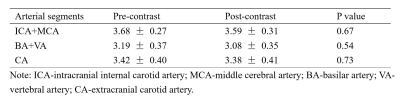
Table 2 Image quality scores
of the images acquired using the 3D intra- and extra-cranial arterial vessel
wall joint imaging with (post-contrast) and without (pre-contrast) contrast
agent.