0352
Decision Curve Analysis for Prostate Biopsy using MRI with or without Dynamic Contrast Enhancement1Radiology, NYU School of Medicine, New York, NY, United States
Synopsis
Prostate MRI with dynamic contrast enhancement (DCE) is controversial with growing interest in noncontrast (NC) MRI. Decision curve analyses performed on data from two contemporary studies identified ranges of high grade cancer probability thresholds at which DCE had the highest net benefit. DCE MRI has the most benefit in moderate or moderate-high risk threshold ranges, thought to vary based on the study differences in disease prevalence, reference standard, and the presence or absence of additional DCE reconstruction images. The risk ranges in which NC versus DCE MRI optimize net benefit may help inform the best clinical use of prostate MRI.
Introduction:
Prostate MRI with dynamic contrast enhancement (DCE) for the detection of prostate cancer is somewhat controversial, with growing interest in noncontrast (NC) MRI. However, the health benefit of DCE versus NC MRI may vary based on the risk threshold at which biopsy is desired, given the morbidity of biopsy and prostate cancer treatment. We compared the net benefit of various diagnostic options over a range of high grade cancer probability thresholds using two contemporary papers.Methods:
Decision curve analysis1 was performed on data from two studies representing patient populations with differing prevalence of high grade prostate cancer undergoing 3T prostate MRI: a) “Study 1” with 343 patients/lesions from 2013-2015 with prevalence reflective of a routine population with low to intermediate clinical risk of high grade prostate cancer, and DCE containing additional golden-angle radial sparse parallel (GRASP) MRI images using an MRI-ultrasound fusion biopsy reference standard2 and b) “Study 2” with 163 patients with 651 lesions from 2012-2015 with standard DCE MRI and a prostatectomy reference standard with high risk of clinically significant prostate cancer.3 We compared the net benefit of five distinct diagnostic options: biopsy none, biopsy all, biopsy PI-RADS ≥3 lesions (not requiring contrast), biopsy PI-RADS ≥4 lesions determined using only NC sequences, and biopsy PI-RADS ≥4 lesions adding DCE MRI. High grade prostate cancer was defined as Gleason Score ≥7.Results:
In Study 1, of 343 lesions, 4, 128, 79, 75, and 57 lesions were PI-RADS 1 through 5 of which 0 (0%), 2 (2%), 9 (11%), 37 (49%), and 42 (74%) were high grade cancer, respectively, for a lesion cancer prevalence of 26%. 10 peripheral zone lesions initially given a PI-RADS 3 were upgraded to a PI-RADS 4 based on DCE with GRASP; 3 (30%) of these were high grade cancer. In Study 2, of 651 lesions, 70, 115, 305, and 161 were PI-RADS 2 through 5 of which 11 (16%), 38 (33%), 215 (71%), and 147 (91%) were high grade cancer, respectively, for a lesion cancer prevalence of 63%. 87 peripheral zone lesions initially given a PI-RADS 3 were upgraded to a PI-RADS 4 based on DCE; 47 (54%) of these were high grade cancer.
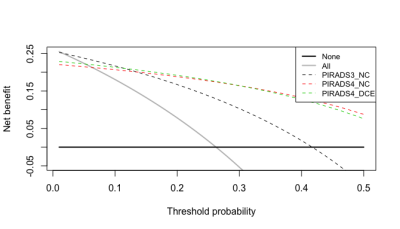
Decision curve analyses results are displayed in the Figures. For Study 1 with low to intermediate disease prevalence (Figure 1): for patients with a very low probability threshold (0-2%) for high grade cancer at which they desire biopsy, a “biopsy all” strategy had the highest net benefit, while patients with a low threshold (2-11%) benefitted the most when biopsying all PI-RADS ≥3 lesions, which would not require MRI contrast. For patients with a moderate threshold (11-30%), biopsy of only PI-RADS ≥4 lesions on DCE MRI using GRASP had the highest benefit; with a high probability threshold (≥30%), biopsy of PI-RADS ≥4 lesions using only NC MRI had the highest benefit.
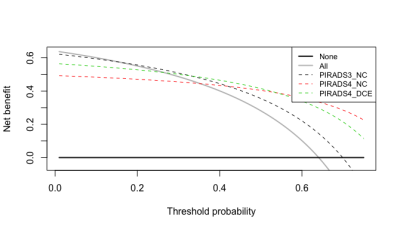
In Study 2 with high disease prevalence (Figure 2): for patients with a low probability threshold (0-15%), a “biopsy all” strategy had the highest net benefit, while patients with a moderate threshold (16-33%) benefitted the most from biopsy of all PI-RADS ≥3 lesions, which would not require MRI contrast. For patients with a moderate-high threshold (34-54%), biopsy of only PI-RADS ≥4 lesions using DCE MRI had the highest benefit; with a high probability threshold (>54%), biopsy of PI-RADS ≥4 lesions using only NC MRI had the highest benefit.
Discussion:
These results identify discrete ranges of high grade cancer risk thresholds at which decision makers would generate the highest net benefit from adding intravenous contrast to prostate MRI, based on underlying pretest probability of clinically significant prostate cancer. In Study 1 and Study 2, the risk threshold ranges of 11-30% and 33-54%, respectively, were most likely to optimize net benefit with use of DCE MRI. The differences in these two study designs likely influenced the range discrepancies. For example, Study 1 used a reference standard of MRI-ultrasound fusion biopsy, while Study 2 used prostatectomy, and GRASP imaging in Study 1 may affect the performance characteristics compared with other DCE sequences.Conclusion:
The comparative net benefit of prostate MRI with or without contrast varies over decision-makers’ risk thresholds and the technique may best be tailored based on clinical risk estimates and patient preferences. DCE MRI with GRASP and standard DCE MRI may be most relevant in patients with moderate and moderate-high risk thresholds for preferring biopsy, respectively. As a supplemental clinical risk assessment for high-grade prostate cancer, MRI technique tailored to the clinical scenario may improve testing efficiency and utility.Acknowledgements
No acknowledgement found.References
1. Vickers AJ, Elkin EB. Decision curve analysis: a novel method for evaluating prediction models. Medical Decision Making. 2006 Nov-Dec;26(6):565-74.
2. Rosenkrantz AB, Babb JS, Taneja SS, Ream JM. Proposed Adjustments to PI-RADS Version 2 Decision Rules: Impact on Prostate Cancer Detection. Radiology. 2017 Apr;283(1):119-129.
3. Greer MD, Shih JH, Lay N, et al. Validation of the Dominant Sequence Paradigm and Role of Dynamic Contrast-enhanced Imaging in PI-RADS Version 2. Radiology. 2017 Jul 19:161316.
Figures