0348
How Fast is “Fast MRI” for Breast Cancer Screening?Emily F. Conant1, Arijitt Borthakur1, Mitchell D. Schnall1, and Susan P. Weinstein1
1Department of Radiology, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States
Synopsis
We compare the scan and total study times from a newly implemented abbreviated MR protocol (AP) for breast cancer screening consisting of localizer, T2-STIR, and single pair of pre- and post-contrast 3D T1 sequences to similar times from our full MRI screening protocol. A retrospective analysis was performed using scan time data obtained from image dicom files as well as data from the Radiology Information System (RIS) for technologist activity times to determine the variance between the two protocols. The results of this study will help guide operational value improvements and estimates for appropriate pricing for the newly implemented AP for breast cancer screening.
Objective
To compare total study time as well as sub-components from a newly-implemented abbreviated protocol (AP) for MRI breast cancer screening with those from a full breast MRI screening protocol.Background
Mammography is the only screening test which has been shown to reduce breast cancer mortality (1). However, the sensitivity of screening mammography is known to be limited by increasing breast density due to masking of cancers by dense breast tissue. In addition, increasing breast density is associated with an increasing risk of developing breast cancer. Presently, over 50% of U.S. states have implemented breast density legislation to notify women about their individual breast density and the possible need for supplemental screening to improve cancer detection–most often with whole breast ultrasound. However, it is well known that breast MRI is more sensitive in detecting breast cancers than mammography, ultrasound, or the combination of mammography and ultrasound (2). Unfortunately, standard breast MRI is expensive and therefore is currently limited to women with a lifetime risk of >20%. Recently, an abbreviated protocol (AP) for MRI breast cancer screening has been developed and has been shown to have excellent sensitivity and specificity (3). With significantly fewer imaging sequences, the AP is expected to increase patient throughput and therefore significantly reduce imaging costs. Here we evaluate the study times of our AP and compare it to our full MR protocol for breast cancer screening.Methods
This project was undertaken as a Quality Improvement Initiative and received exemption by our Institutional Review Board. A modification of the abbreviated protocol (AP) of Kuhl et al. (3) was implemented at our institution as a supplemental screening study for women with mammographically dense breasts. Currently, we include a T2 STIR sequence to investigate the added diagnostic value, understanding that the T2 adds considerable time. For this analysis, we conducted a retrospective study of a subset of patients who underwent contrast enhanced breast MRI for breast cancer screening from September 2016-August 2017 with either the abbreviated (N=70) or full (N=736) MRI protocols. Patients had either normal or benign screening mammograms and for those undergoing the AP screen, their most recent mammogram must have been reported as BI-RADS density b or c (heterogeneously or extremely dense) (4). Statistical analyses (ANOVA, Q-Q plots, etc.) were performed in JMP Pro 13 (SAS, Cary, NC). We first calculated the total expected scan time by summing the time of acquisition for each imaging series under each protocol (Figure 1). Using code written in Python, the actual scan time was obtained for each patient by calculating the difference of the DICOM time stamps and recorded in a CSV file for analyses. Finally, the time from opening and closing a patient exam by the tech was obtained by searching the RIS using mPower (Nuance Inc, Burlington, MA) and was recorded as total study time. Subtracting actual scan time from total scan time results in the total tech activity time, of which there are scan-related activities (processing MIPs, injecting) and non-scan-related activities e.g. removing patient.Results
On average the actual scan time for an AP screen was 17.5 mins which is significantly faster than the full protocol time of 28.8 mins (difference = 11.3 mins; p<0.0001). Scan-related tech activity time was ~5 minutes greater for the AP screen and most likely due to image processing activities that can be absorbed into the longer actual scan time for the FULL screen. Additional time measurement studies will be performed to fully explain this observation and help guide operational efficiency improvements for AP scans. The AP screen has a 1.4x higher flow rate (1/total study time) because the FULL screen’s non-scan related activity time was 72% more than the AP screen’s and could potential be reduced with lean methods.Conclusions
Implementation of the AP for breast cancer screening can significantly reduce scan times and improve patient throughput. We recognize that the T2 sequence comprises almost 50% of the expected scan time and may in the future be removed from the protocol pending review of outcomes. Since the AP screen is offered as a supplemental screen that currently is not reimbursed by insurance, we will use this data and additional cost information to estimate scheduling parameters, appropriate pricing and to target areas for operational improvements.Acknowledgements
We thank Bruno Barufaldi, PhD, Thomas Chiang, and Donovan Reid for help with data extraction. This work was performed at a NIBIB Biomedical Technology Research Center under Grant No. P41 EB015893.References
- Tabár L, Vitak B, Chen TH, Yen AM, Cohen A, Tot T, Chiu SY, Chen SL, Fann JC, Rosell J, Fohlin H, Smith RA, Duffy SW. Swedish two-county trial: impact of mammographic screening on breast cancer mortality during 3 decades. Radiology 2011;260(3):658-663.
- Kuhl CK, Schrading S, Weigel S, Nüssle-Kügele K, Sittek H, Arand B, Morakkabati N, Leutner C, Tombach B, Nordhoff D, Perlet C, Rieber A, Heindel W, Brambs HJ, Schild H. [The "EVA" Trial: Evaluation of the Efficacy of Diagnostic Methods (Mammography, Ultrasound, MRI) in the secondary and tertiary prevention of familial breast cancer. Preliminary results after the first half of the study period]. Rofo 2005;177(6):818-827.
- Kuhl CK, Schrading S, Strobel K, Schild HH, Hilgers RD, Bieling HB. Abbreviated breast magnetic resonance imaging (MRI): first postcontrast subtracted images and maximum-intensity projection-a novel approach to breast cancer screening with MRI. J Clin Oncol 2014;32(22):2304-2310.
- Sickles E, D’Orsi C, Bassett L, et al. Mammography. In: ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System Reston, VA: American College of Radiology; 2013.
Figures
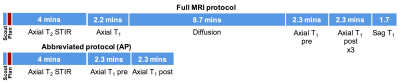
Figure 1: Expected scan times are 26 minutes for the
full protocol and 9.5 minutes for the abbreviated protocol (AP). Not shown are processing times for subtraction and maximum intensity
projection (MIP) images that could be performed by the tech, for example, while
a scan is running.
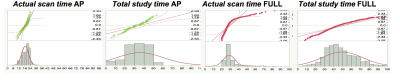
Figure 2: Normal quantile (Q-Q) plots (top) and histograms
(bottom) for abbreviated (AP) and complete (FULL) screens scaled 0-100 minutes.
Q-Q plots show a fairly good assumption of normality
in the data except in Actual scan time FULL protocol data.
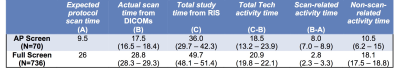
Table 1:
Average times in minutes (±95% CI).