0296
SAR estimation error due to body model mismatch for fetal imaging at 3 Tesla1Fetal-Neonatal Neuroimaging and Developmental Science Center, Boston Children's Hospital, Boston, MA, United States, 2A.A. Martinos Center for Biomedical Imaging, Department of Radiology, Massachusetts General Hospital, Charlestown, MA, United States, 3Harvard Medical School, Boston, MA, United States, 4Harvard-MIT Division of Health Sciences and Technology, Massachusetts Institute of Technology, Boston, MA, United States, 5Department of Electrical Engineering and Computer Science, Massachusetts Institute of Technology, Cambridge, MA, United States, 6Institute for Medical Engineering and Science, Massachusetts Institute of Technology, Cambridge, MA, United States
Synopsis
RF safety concerns have been raised for both the mother and the fetus for 3 T fetal MRI. Parallel transmission can address these concerns by reducing the maternal and fetal SAR however it also relies on one or more body models to predict that individual’s local SAR. In this work, we assess the range of error incurred when various pregnant or non-pregnant models are used to predict SAR in pregnant patients. We model the degree of over or underestimation of SAR in 56 combinations of model/patient and find a maximum SAR under/over-estimation of 59%/142%.
Target Audience
MR physicists and clinicians interested in RF safety of 3 T fetal imaging.Introduction
3 T MRI is advantageous for fetal imaging over the more established 1.5 T protocols due to improved SNR. However, there are some concerns over the RF safety of both the mother and the fetus at this field strength, as indicated by simulation studies1,2 and animal experiments3. Parallel RF transmission (pTx)4 has the potential to address these concerns by reducing the specific absorption rate (SAR) of both the mother and the fetus5,6. However, the management of SAR is complicated with pTx systems. Realistic electromagnetic body models are used to estimate and monitor local SAR to avoid potential hot spots. The use of body models in SAR monitoring raises the question of how well the model used represents the patient on the table. This is particularly troubling if non-pregnant body models are used in a fetal imaging study. In this work, the amount of SAR estimation error due to body model mismatch in fetal imaging is analyzed for a 2-channel birdcage coil model driven in standard and RF shimming modes using various pregnant and non-pregnant body models.Methods
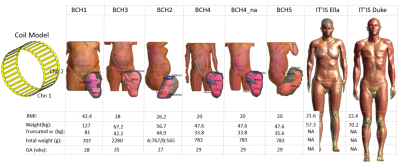
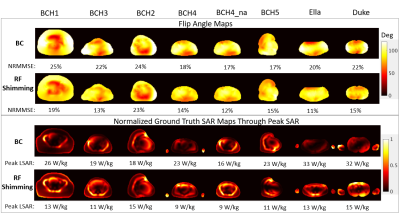
EM simulations: 6 truncated pregnant body models (BCH)7 and 2 full body non-pregnant body models (IT’IS foundation, Zurich, Switzerland) are simulated inside a 2-channel 32-rung birdcage coil model (Figure.1). The body models BCH4, BCH5 and BCH4_na are created from the same person, in supine and left lateral positions and without the arms. All models are placed inside the coil in the head-first position. RF pulse design: RF pulses to drive the coil model are designed for a single axial (maternal) slice through the fetal brain with the target of a 90° average flip angle throughout the slice. A sinc shaped waveform of 3 ms duration and time bandwidth product of 2 is used. For the birdcage (BC) mode, the two channels have a fixed phase difference and the same amplitude, scaled differently across different body models. For the RF shimming pulses, a SAR constrained high-flip angle RF pulse design algorithm is used to optimize the complex weights for each channel8 to simultaneously reduce SAR and improve flip angle uniformity. SAR calculation: For each body model, the peak local SAR created by the designed RF pulse is estimated using all the body models. The SAR estimated using the corresponding body model for which the RF pulse was designed is called the ground truth SAR. The estimated SAR values are divided by the ground truth SAR to calculate the under- and over-estimation factors in Figure.2.Results/Discussion
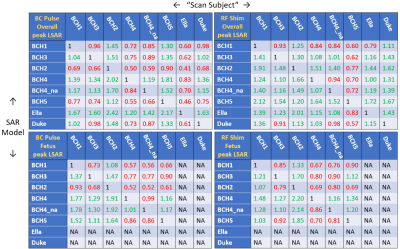
Figure.2 shows the estimation error tables of overall (mother+fetus) and fetal peak local SAR for both BC and RF shimming modes. An entry of 1.2 corresponds to 20% overestimation and 0.7 corresponds to 30% underestimation. For BC mode: both the overall and the fetal peak local SAR of the lowest BMI models (BCH4 and BCH4_na) are usually underestimated by the higher BMI models. Overall SAR of the models in left lateral position (BCH2 & BCH5) are always overestimated by supine position models. The model with arms at the side (BCH4) overestimates the overall SAR and underestimates the fetal SAR of the model without the arms (BCH4_na). For RF shimming mode: Pairs of models both overestimate the SAR of each other in many cases (explained by RF pulses for each model being different). The model with arms at the side (BCH4) underestimates the overall SAR and overestimates the fetal SAR of the model without the arms (BCH4_na), and the models in the left lateral position overestimate the overall SAR of the models in supine position, both of which are opposite to what happens in BC mode. Overall SAR of BCH5 is underestimated by all models. Both: There is no one-to-one relationship between the under- and over-estimation patterns of the fetal and overall SAR. The non-pregnant female body model overestimates overall SAR in all cases except for BCH5 in RF shimming. The male body model underestimates overall SAR in approximately half of the cases.Conclusion
Significant variation in the SAR estimation errors due to body model mismatch was observed across various body models, different RF pulses and the fetal and overall SAR. The results indicate that either patient specific body models should be used or several cases including various pregnant body models and RF configurations should be combined into a worst-case scenario. Future work will include a statistical analysis of several RF shimming configurations for each model and the study of SAR estimation errors in practice in the standard mode of operation.Acknowledgements
This work was supported by R01 EB017337, R01 EB006847, P41EB015896, U01 HD087211, Siemens MR, and the Sim4Life support group.References
1-Hand JW, Li Y, Hajnal JV. Numerical study of RF exposure and the resulting temperature rise in the foetus during a magnetic resonance procedure. Phys Med Biol. 2010;55: 913-30.
2-Nagaoka T, Saito K, Takahashi M, Ito K, Watanabe S. Anatomically realistic reference models of pregnant women for gestation ages of 13, 18, and 26 weeks. 30th Annual International Conference of the IEEE Engineering in Medicine and Biology Society 2008 Aug 20 (pp. 2817-2820).
3-Cannie M, De Keyzer F, Van Laere S, de Mey J, Fourneau, De Ridder F, Willekens I, Jani JC. Potential Heating Effect in the Gravid Uterus by Using 3-T MR Imaging Protocols: Experimental Study in Miniature Pigs. Radiology. 2016;279(3):754-61.
4-Katscher U, Börnert P, Leussler C, Van Den Brink JS. Transmit sense. Magn Reson Med. 2003;49:144-50.
5-Murbach M, Neufeld E, Samaras T, Corcoles J, Robb FJ, Kainz W, Kuster N. Pregnant women models analyzed for RF exposure and temperature increase in 3T RF shimmed birdcages. Magn Reson Med 2016;77:2048-2056.
6-Yetisir F, Abaci Turk E, Guerin B, Grant PE, Wald LL, Adalsteinsson E. Potential of Parallel Transmission for Fetal Imaging in Reducing SAR and Mitigating Flip Angle Inhomogeneities: A Simulation Study at 3T. In Proceedings of the 25th Meeting of ISMRM, Honolulu, Hawaii, USA, 2017. Abstract 4823.
7-Abaci Turk E, Yetisir F, Gagoski BA, Guerin B, Copeland N, Wald LL, Adalsteinsson E, Grant PE. Safety of 3T MRI Scan for Pregnant Women: Effect of Maternal Size, Maternal Position and Twin Pregnancy. In Proceedings of the 25th Meeting of ISMRM, Honolulu, Hawaii, USA, 2017. Abstract 4810.
8-Yetisir F, Guerin B, Poser BA, Wald LL, Adalsteinsson E. Impact of RF-shimming on the uniformity and specific absorption rate of spin-echo imaging at 7 Tesla. In Proceedings of the 23rd Meeting of ISMRM, Toronto, ONtario, Canada, 2015. Abstract 0920.
Figures