0131
Whole body functional and anatomical MRI: Accuracy in staging and interim response monitoring of Childhood and Adolescent Hodgkin’s Lymphoma compared to multimodality conventional imaging1Centre for Medical Imaging, University College London, London, United Kingdom, 2Cancer Research UK and UCL Cancer Trial Centre, University College London, London, United Kingdom, 3Institute of Nuclear Medicine, University College London Hospital, London, United Kingdom, 4Department of Paediatric Haemato-oncology, University College London Hospital, London, United Kingdom
Synopsis
Whole-body MRI (WB-MRI) offers an alternative non-ionising radiation technique to current gold-standard imaging, 18F-FDG PET-CT, for assessment of paediatric and adolescent Hodgkin's lymphoma (HL).
In this work we prospectively evaluated WB-MRI, including diffusion-weighted-imaging (DWI), for initial staging and early interim response monitoring in 50 paediatric HL patients.
WB-MRI with DWI has reasonable intrinsic diagnostic accuracy for nodal and extra-nodal staging of paediatric HL but it fails to achieve full concordance with standard imaging for all disease sites in minority of patients.
WB-MRI has reasonable accuracy for interim response classification but tends to underestimate disease response, particularly in extra-nodal disease sites.
Introduction
Combined Positron emission tomography/computed tomography (18F-FDG PET-CT) remains the primary imaging modality for staging and interim response monitoring of paediatric lymphomas, although exposes patients to significant doses of ionising radiation [1]. One particular strength is the functional metabolic information afforded by the 18F-FDG PET component, which supplements anatomical imaging Whole-body MRI (WB-MRI) offers an alternative non-ionising radiation technique [2] providing high resolution anatomical images. Furthermore, diffusion- weighted-imaging (DWI) could provide functional information [3] [4], with data reporting a significant negative correlation between DWI’s apparent-diffusion-coefficient (ADC), and 18F-FDG PET-CT’s maximum-standardised-uptake-value (SUVmax) [5]. The purpose of this study was to investigate prospectively the concordance between WB-MRI and a composite reference standard including 18F-FDG PET-CT, for initial staging and interim response monitoring in paediatric and adolescent Hodgkin’s lymphoma [HL].Material and Methods
Fifty patients (39 male, median age 16, range 5-19) with confirmed diagnosis of HL underwent 1.5 T WB-MRI at initial staging and following 2-3 chemotherapy cycles in addition to conventional 18F-FDG PET–CT and CT (Figure 1). The primary-reference-standard disease status at 32 (18 nodal, 14 extra-nodal) sites and Ann-Arbor stage was assigned by a multidisciplinary-team (MDT) committee based on all clinical/ imaging data using the EURONET trial criteria (nodal-positivity: long-axis > 2cm and/or focal 18F-FDG uptake above background) [6]. WB-MRI was read in consensus by 2 radiologists blinded to conventional imaging. The disease status for the same 32 sites were derived using a combination of size (long-axis > 2cm) and ADC measurements (using predefined cut-offs for positivity) and Ann-Arbor stage was assigned. Extra-nodal disease was assessed as previously described [7]. Nodal response was defined using nodal volume and SUVmax changes for 18F-FDG PET-CT and nodal volume [6] and pre-defined ADC changes for WB-MRI. Extra-nodal response was assessed based on qualitative changes of 18F-FDG PET-CT and WB-MRI signal characteristics. Given the potential limitations of the primary-reference-standard, an enhanced-reference-standard was created by a multi-disciplinary consensus-committee-panel, unblinded to all imaging and using long-term patient follow-up data. Initially, the panel corrected the anatomical-boundaries-discrepancies (i.e. discrepancies due to differences in radiologists’ description of the disease sites’ anatomical locations) between the primary-reference-standard and WB-MRI. Thereafter, perceptual errors (misinterpretations by the original MDT radiologists) and technical failures (limitations of imaging techniques) were corrected for the primary-reference to derive the “enhanced-reference-standard”. Finally, WB-MRI data was corrected for readers’ perceptual errors to define the theoretical best-performance of the technique. For staging, agreement between WB-MRI (before/after correction of perceptual errors) and the primary- and enhanced-reference-standards was expressed as percentage-concordance for each of the 32 disease sites, and kappa-statistics. Absolute-agreement-rate, true-positive-rate (TPR) (sensitivity) and false-positive-rate (FPR) (1-specificity) for nodal and extra-nodal disease sites were derived for WB-MRI (before /after correction of perceptual errors) against the primary- and enhanced-reference-standards. Agreement for Ann-Arbor staging and interim response evaluation were summarized in terms of frequency, percentages and kappa-statistics.Results
Per-patient concordance rate for each analysis shown in Figure 2. After removal of WB-MRI perceptual errors, the discordance rates against enhanced-reference-standard for all sites, nodal and extra-nodal sites were 18% (90% CI exact 9.7%-29.3%), 16% (90% CI exact 8.2%-27.0%) and 4% (90% CI exact 0.7%-12.1%) respectively. Absolute-agreement-rate, TPR, FPR and Cohen’s kappa statistic for nodal/extra-nodal disease sites for each analysis are shown in Figure 3. Following removal of WB-MRI perceptual errors, the TPR, FPR and kappa agreement were 97%, <1% and 0.97 (95% CI: 0.95-0.99) for nodal and 95%, 0% and 0.97 (95% CI: 0.93-1.00) for extra-nodal assessment compared to enhanced-reference-standard. After removal of the WB-MRI perceptual errors concordance was achieved in 48/50 (96%) patients for Ann-Arbor staging (Kappa 0.94 (95% CI: 0.85-1.00)) (Figure 4). Two patients under-staged by WB-MRI compared to enhanced-reference-standard (Figure 5). Thirty-eight patients had all interim scans following 2-3 cycles of chemotherapy. For interim response, WB-MRI agreed with primary-reference-standard in 25/38 patients (66%), underestimating response in 11 (29%), and overestimating response in 2 (5%) patients (Kappa 0.28, 95% CI: 0.02-0.54). WB-MRI agreed with primary-reference-standard response classification in 126/143 (88%) of nodal sites and 17/26 (66%) extra-nodal sites.Discussion and Conclusion
WB-MRI with DWI has reasonable intrinsic diagnostic accuracy for nodal and extra-nodal staging of paediatric HL. However, in a substantial minority of patients it fails to achieve full concordance with standard imaging for all disease sites, which may have implications for treatment-planning such as targeted radiotherapy for involved nodal stations. WB-MRI has reasonable accuracy for interim response classification but tends to underestimate disease response, particularly in extra-nodal disease sites. Overall, although promising, WB-MRI with DWI cannot currently replace standard imaging investigations in pediatric HL and further technical improvements are required.Acknowledgements
This study was supported by funding from Cancer Research UK, project number CRUK ASC 12707.
AL was supported by a Cancer Research UK/ Engineering and Physical Sciences Research Council (CRUK/EPSRC) award (C1519/A10331 and C1519/A16463) from the University College London/King’s College London (UCL/KCL) Comprehensive Cancer Imaging Centre (CCIC).
SAT is an NIHR senior investigator.
This work was undertaken at the Biomedical Research Centre (BRC), University College Hospital London (UCLH), which received a proportion of the funding from the National Institute for Health Research (NIHR). The views expressed in this publication are those of the authors and not necessarily those of the UK Department of Health.
References
[1] Uslu L, Doing J, Link M, et al. Value of 18F-FDG PET and PET/CT for Evaluation of Pediatric Malignancies. J Nucl Med.2015;56(2):274-286.
[2] Greer MC, Voss SD, States LJ. Pediatric Cancer Predisposition Imaging: Focus on Whole-Body MRI. Clin Cancer Res. 2017 Jun 1;23(11):e6-e13.
[3] van Ufford HM, Kwee TC, Beek FJ, et al. Newly diagnosed lymphoma: initial results with whole-body T1-weighted, STIR, and diffusion-weighted MRI compared with 18F-FDG PET/CT. Am J Roentgenol. 2011;196(3):662-669.
[4] Kwee T, Ludwig I, Uiterwaal CS, et al. ADC measurements in the evaluation of lymph nodes in patients with non-Hodgkin lymphoma: feasibility study. Magn Reson Mater Phy. 2011;24(1):1-8.
[5] Punwani S, Taylor SA, Saad ZZ, et al. Diffusion-weighted MRI of lymphoma: prognostic utility and implication for PET/MRI? Eur J Nuc Med Mol Imaging.2013;40(3):373-385.
[6] Körholz D, Wallace H, Landman-Parker J (2006) EuroNet-Paediatric Hodgkin’s Lymphoma Group, First international Inter-Group Study for classical Hodgkin’s Lymphoma in Children and Adolescents, Radiotherapy Manual. https://www.skion.nl/workspace/uploads/euronet-phl-c1_workingcopy_inkl_amendm06_mw_2012-11-14_0.pdf
[7] Punwani S, Taylor SA, Bainbridge A, et al. Pediatric and adolescent lymphoma: comparison of whole-body STIR half-Fourier RARE MR imaging with an enhanced PET/CT reference for initial staging. Radiology. 2010;255(1):182-190.
Figures
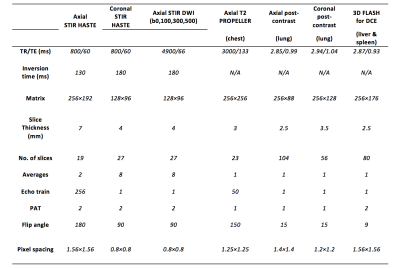
Figure 1: Whole-body MRI sequence parameters
TR: Repetition time TE: Echo time PAT: Parallel acquisition technique STIR: Short tau inversion recovery HASTE: Half-Fourier single shot turbo spin echo DWI: Diffusion weighted imaging FLASH: Fast low angle shot technique DCE: Dynamic contrast enhanced PROPELLER: Periodically rotated overlapping lines with enhanced reconstruction
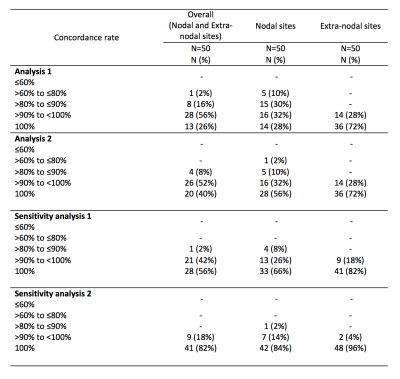
Figure 2: Per patient concordance rate for each analysis
Analysis 1: Comparison between WB-MRI and primary reference standard before correction of simple anatomical boundaries labelling discrepancies Analysis 2: Comparison between WB-MRI and primary reference standard following correction of simple anatomical boundaries labelling discrepancies Sensitivity analysis 1: Comparison between WB-MRI and enhanced reference standard (after removal of perceptual and technical errors in the primary reference standard) Sensitivity analysis 2: Comparison between WB-MRI and enhanced reference standard following removal of WB-MRI perceptual errors
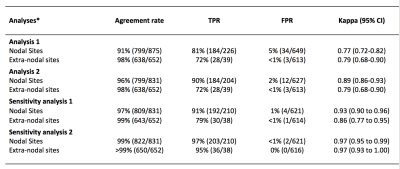
Figure 3: True positive rate, false positive rate, agreement rate and kappa for nodal / extra-nodal staging
Analysis 1: Comparison between WB-MRI and primary reference standard before correction of simple anatomical boundaries labelling discrepancies Analysis 2: Comparison between WB-MRI and primary reference standard following correction of simple anatomical boundaries labelling discrepancies Sensitivity analysis 1: Comparison between WB-MRI and enhanced reference standard (after removal of perceptual and technical errors in the primary reference standard) Sensitivity analysis 2: Comparison between WB-MRI and enhanced reference standard following removal of WB-MRI perceptual errors TPR: true positive rate; FPR: false positive rate; CI: confidence interval
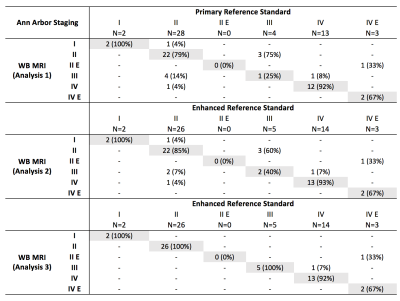
Figure 4: Ann Arbor staging agreement
Analysis 1: Comparison between WB-MRI and primary reference standard Analysis 2: Comparison between WB-MRI and enhanced reference standard before removal of WB-MRI perceptual errors Analysis 3: Comparison between WB-MRI and enhanced reference standard following removal of WB-MRI perceptual errors
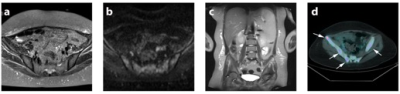
Figure 5: Example of WB-MRI technical error.
False negative WB-MRI technical error resulting in under-staging of a fifteen year old female patient with multi-focal bone marrow involvement; (a) axial STIR-HASTE, (b) DWI b500 and (c) coronal STIR-HASTE MRI show no discernable bone marrow abnormality. (d) Fused 18F-FDG PET-CT however demonstrates multi-focal bone marrow metastasis (arrows).