0130
Whole-Body MRI for Metastatic Cancer Detection using T2-Weighted Imaging with Fat and Fluid Suppression1Radiology, UT Southwestern Medical Center, Dallas, TX, United States, 2Internal Medicine, UT Southwestern Medical Center, Dallas, TX, United States, 3Kidney Cancer Program, Simmons Comprehensive Cancer Center, UT Southwestern Medical Center, Dallas, TX, United States, 4Advanced Imaging Research Center, UT Southwestern Medical Center, Dallas, TX, United States
Synopsis
Whole-body diffusion with background suppression (DWIBS) has increased sensitivity and specificity for metastatic cancer detection. However, DWIBS using echo-planar readout suffers from geometric distortions due to large B0 inhomogeneities associated with large FOV, used in whole-body MRI. Additionally, DWIBS suffers from low spatial resolution and long scan times due to low signal to noise ratio. In this work, we developed an alternative WB-MRI technique at 3T using fast, high-resolution and high-SNR T2-weighted imaging with simultaneous fat and fluid suppression, called DETECT. Patient studies show that, DETECT is time-efficient, robust, and generates distortion-free images with good lesion conspicuity, compared to DWIBS.
Introduction
Whole-body diffusion weighted imaging with background suppression (DWIBS) have shown improved sensitivity and specificity for metastatic cancer detection1-3. However, DWIBS images, acquired using echo-planar (EPI) readout, suffer from geometric distortions due to large B0 inhomogeneities within the large fields of view used in whole-body MRI (WB-MRI). Additionally, DWIBS images are often acquired with reduced spatial resolution and multiple signal averages due to low signal to noise ratio (SNR), resulting in prolonged scan times. While the higher SNR can be achieved at 3T (compared to 1.5T), the more pronounced B0 inhomogeneities at 3T lead to increased geometric distortions, often resulting in nondiagnostic images. Thus, the purpose of this work was to develop a WB-MRI technique at 3T using fast, high-resolution and high-SNR T2-weighted imaging with simultaneous fat and fluid suppression for metastatic cancer detection.Methods
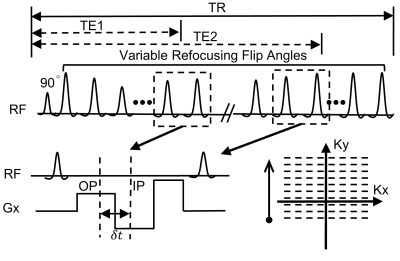
A single-shot turbo-spin-echo (SShTSE) sequence was combined with mDixon for fat suppression4 and dual-echo based subtraction for fluid suppression5, and was called Dual-Echo T2-weighted acquisition for Enhanced Conspicuity of Tumors (DETECT). This sequence generates 4 sets of images in a single repetition: in-phase (IP) and out-of-phase (OP) images at a short TE and a long TE (Fig.1). The short-TE IP/OP images were reconstructed with a standard mDixon reconstruction and the long-TE IP/OP images were generated with a shared-field-map mDixon reconstruction using the field-map from the short TE, for robust fat/water separation5. The water-only images between the two TEs were subtracted using complex subtraction for fluid suppression5. All imaging was performed on a 3T Philips Ingenia MR scanner with IRB approval and written informed consent. WB-MRI with DETECT was compared against DWIBS in 3 healthy volunteers and 5 patients with known metastatic renal cell carcinoma (mRCC). Five stations were typically scanned to cover the whole body from head to knees. The typical acquisition parameters of the DETECT included: coronal orientation; FOV = 300×300 mm2 (head), 320×520 mm2 (body); slice thickness = 5 mm; Resolution = 1.2×1.2 mm2 (head), 1.3×1.8 mm2 (body); TE1/TE2 = 80/450 ms; acquisition time = 1 min/station for approximately 50 slices. The thoracic and abdominal regions were acquired in four, 15-second breathheld acquisitions each. DWIBS used the same parameters except: b = 0 (NSA=1), 800 s/mm2 (NSA=6); 3 directions; Resolution = 3.5×3.5 mm2; acquisition time = 3:09 for head and 3:20 min/station for the body. In one healthy volunteer, axial DWIBS images were also acquired with a scan time of 3:09 for head and 5:15 min/station for the body.Results
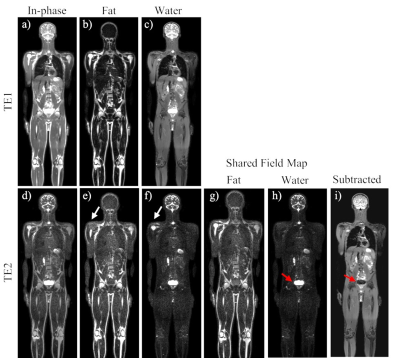
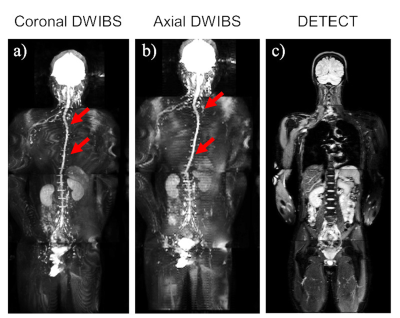
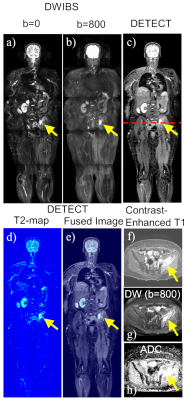
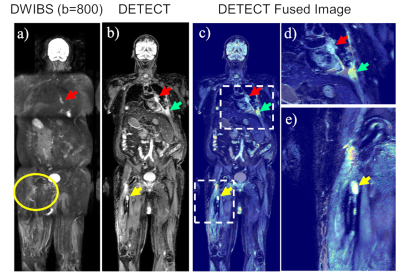
Figure 2 illustrates WB-MRI with DETECT in a healthy volunteer with robust fat/water separation at the short TE (Figs. 2a-c). Fat/water swaps (white arrows, Figs. 2e,f) at the long TE due to the reduced SNR were corrected by the shared-field-map mDixon reconstruction (Figs. 2g, h); Fluid signal (e.g. CSF) was successfully suppressed in the subtracted image (Fig. 2i). Figure 3a illustrates significant geometric distortion commonly seen in coronal DWIBS acquisition. An attempt to address this challenge (through an axial DWIBS acquisition) resulted in similar distortion, as seen in the coronal reconstructions (Figure 3b). Alternatively, DETECT images in the same subject provided distortion-free images (Fig. 3c) in less than half the acquisition time (6 minutes for DETECT, compared to respectively 14 and 19 minutes for coronal and axial DWIBS). Figure 4 demonstrates images of a patient with known RCC metastasis to the left ilium, where both DETECT and DWIBS images delineate the lesion. The effective T2-map (Fig. 4d), generated with T2 values less than 300 ms, fused with the subtracted DETECT image, provided improved tumor-to-background contrast compared to DETECT and DWIBS. (Fig. 4e). Figure 5 illustrates representative images of another patient with mRCC; while both DWIBS and DETECT images reveal large lesions (e.g. a left hilar lesion, Fig. 5b red, green arrows), the DWIBS images suffer from geometric distortions. In addition, a lesion in the right femur abutting the metallic implant is not visualized on the DWIBS images due to severe image distortion (yellow circle, Fig. 5a), while it is clearly visible on the DETECT images (yellow arrow, Figs. 5b-e).Discussion and Conclusion
We have developed a fast, high-resolution, and high-SNR T2-weighted imaging with uniform, simultaneous fat and fluid suppression (DETECT) for whole-body MRI at 3T. Compared to the commonly used DWIBS, DETECT is time-efficient, robust, and generates distortion-free images with good lesion conspicuity. This robust sequence may serve as an initial screening technique for whole-body cancer imaging, followed by characterization of selected tumors by dedicated functional MR imaging.Acknowledgements
No acknowledgement found.References
1. Klenk C, Gawande R, Uslu L, et al. Ionising radiation-free whole-body MRI versus 18 F-fluorodeoxyglucose PET/CT scans for children and young adults with cancer: a prospective, non-randomised, single-centre study. The lancet oncology 2014;15(3):275-285.
2. Schmidt GP, Reiser MF, Baur-Melnyk A. Whole-body MRI for the staging and follow-up of patients with metastasis. European journal of radiology 2009;70(3):393-400.
3. Takenaka D, Ohno Y, Matsumoto K, et al. Detection of bone metastases in non‐small cell lung cancer patients: Comparison of whole‐body diffusion‐weighted imaging (DWI), whole‐body MR imaging without and with DWI, whole‐body FDG‐PET/CT, and bone scintigraphy. Journal of Magnetic Resonance Imaging 2009;30(2):298-308.
4. Wang X, Greer JS, Pedrosa I, Rofsky NM, Madhuranthakam AJ. Robust abdominal imaging with uniform fat suppression using Dixon based single shot turbo spin echo. In Proceedings of the 24th Annual Meeting of ISMRM. Singapore, 2016. 0573.
5. Wang X, Greer JS, Pinho MC, Lenkinski RE, Madhuranthakam AJ. Volumetric T2-weighted and FLAIR Imaging of Spine with Uniform Fat Suppression in a Single Acquisition. In Proceedings of the 25th Annual Meeting of ISMRM. Honolulu, Hawaii, USA, 2017. 0191.
Figures