0099
Ultrafast Dynamic Contrast Enhanced MRI of the Breast Using DISCO: Are the Quantitative Parameters Helpful in Differentiating between BI-RADS 4 and 5 Subcentimeter Invasive Carcinomas and Benign Lesions?1Department of Radiology, Memorial Sloan Kettering Cancer Center, New York, NY, United States, 2Lenox Hill Radiology, New York, NY, United States, 3Department of Radiology & Biomedical Imaging, University of California, San Francisco, San Francisco, CA, United States, 4Department of Medical Physics, Memorial Sloan Kettering Cancer Center, New York, NY, United States
Synopsis
The quantitative parameters derived from ultrafast dynamic contrast enhanced (UF-DCE) breast MRI using DISCO were analyzed for the assessment of possible utility in the differentiation between subcentimeter invasive carcinoma and benign lesions. Of all these parameters (MS, CER, IAUGC, BAT and Ktrans), BAT was the only parameter that predicted subcentimeter invasive carcinoma. We believe the significantly shorter BAT for subcentimeter invasive carcinomas is congruent with the known pathophysiology of cancer and may reflect its increased vascularity or shunt formation. BAT can be a complementary parameter to conventional steady-state DCE MRI, which could further stratify subcentimeter BI-RADS 4 and 5 lesions.
Introduction
Ultrafast dynamic contrast enhanced (UF-DCE) breast MRI using differential sub-sampling with cartesian ordering (DISCO), characterized by high temporal and spatial resolution, enables image acquisition at multiple time points starting simultaneously with the beginning of contrast injection. Quantitative parameters calculated from these images reflect contrast inflow effects and are known to be useful for the differentiation between cancers and benign lesions1-6.
Breast MRI has the highest sensitivity for breast cancer detection. However, it often depicts subcentimeter lesions that result in biopsy recommendations (BI-RADS 4 and 5) of which the majority are benign, resulting in low breast MRI positive predictive value and specificity7-9. This study aims to evaluate the quantitative parameters derived from UF-DCE MRI in differentiating between subcentimeter BI-RADS 4 and 5 invasive carcinomas and benign lesions.
Methods
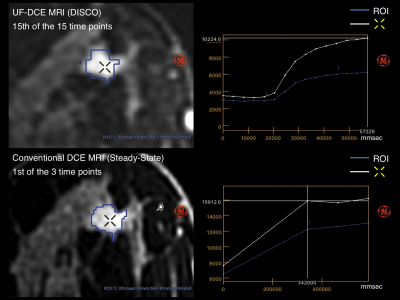
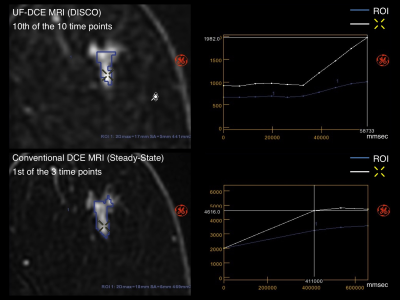
This retrospective Health Insurance Portability and Accountability Act (HIPAA)-compliant study received institutional review board approval. We identified female patients between February-August 2017 with a: 1) UF-DCE MRI with DISCO as part of hybrid protocol with conventional steady-state DCE MRI (Figure 1) and 2) biopsy proven BI-RADS 4, 5 or 6 lesion. BI-RADS 4 and 5 subcentimeter invasive carcinomas and benign lesion were identified as those with a volume<0.523 cm3 (corresponding to a sphere with a diameter of 1cm) using 3D volumetric segmentation. All biopsy-proven BI-RADS 4, 5 and 6 invasive carcinomas and benign lesions were also analysed for a comparison purpose (Figure 2).
All MRI examinations were performed with a 3.0T MRI system (Discovery 750, GE Medical Systems, Waukesha, WI) with a dedicated 16 or 8 channel breast coil. All DCE images were acquired in the axial orientation. After scanning the pre phase for conventional DCE MRI, UF-DCE MR images were acquired continuously 10-15 times during the first 60 sec (temporal resolution of 3.5-6 sec) starting simultaneously with the beginning of contrast injection of 0.1 mmol gadobutrol per kilogram body weight (Gadavist; Bayer Healthcare Pharmaceuticals Inc., Whippany, NJ) at a rate of 2ml/sec with an automatic injector. Following these, conventional 3-phase DCE MR images were acquired continuously three times. The parameters were as follows; UF-DCE MRI using DISCO (TR/TE/FA=3.8/1.7/10°; Reconstructed Matrix, 256×256; FOV, 1.6 × 1.6mm; thickness, 1.6mm; temporal resolution, 3.5-6 sec); conventional DCE MRI (TR/TE/FA=7.9/4.3/12°; Reconstructed Matrix, 512×512; FOV, 1.1 × 1.1mm; thickness, 1.1mm; temporal resolution, ~120 sec).
Using GenIQ Software (GE Healthcare), 3D volumetric segmentation was manually performed for each lesion on the 1st post contrast conventional DCE images and cloned to UF-DCE MRI. Maximum slope (MS), contrast enhancement ratio (CER), initial area under the gadolinium curve (IAUGC), bolus arrival time (BAT) and Ktrans were calculated for UF-DCE MRI. Maximum slope of increase (MSI), signal enhancement ratio (SER), and positive enhancement integral (PEI) were calculated for conventional DCE MRI.
Wilcoxon signed rank sum test and t-tests was used to compare these parameters between invasive carcinomas and benign lesions. To evaluate the diagnostic accuracy of each parameter to predict invasive carcinoma, areas under the receiver operating characteristic (ROC) curve (AUC) were calculated. AUC values were evaluated as follows; 1.0>AUC≥0.9, high accuracy; 0.9>AUC≥0.7, moderate accuracy; 0.7>AUC>0.5, low accuracy. P values less than 0.05 were considered statistically significant. All analyses were performed using SAS 9.4 (The SAS Institute, Cary, NC).
Results
In total, 190 BI-RADS 4,5 or 6 MRI examinations were included and 237 lesions (invasive carcinomas, 141; benign lesions, 96) were identified (cohort A). Of these, there were 103(43.5%) BI-RADS 4 and 5 subcentimeter lesions, 21 invasive carcinomas and 82 benign lesions (cohort B) (Figure 2).
Results of the analysis are shown in Figure 3. In both cohorts (A and B), all the parameters presented significant difference between invasive carcinomas and benign lesions. The AUC evaluation for BI-RADS 4 and 5 subcentimeter lesions (cohort B) demonstrated that BAT (UF-DCE MRI parameter) was the only parameter showing AUC>0.7. When all biopsy-proven lesions were included (cohort A), all the UF-DCE MRI parameters presented AUC>0.7 with higher accuracy than SER (conventional DCE MRI parameter) showing AUC=0.763. Representative two cases are shown in Figure 4-5.
Discussion
BAT was the only quantitative UF-DCE MRI parameter that differentiated/predicted subcentimeter invasive carcinomas with moderate accuracy. We believe the significantly shorter BAT for subcentimeter invasive carcinomas is congruent with the known pathophysiology of cancer and may reflect its increased vascularity10, 11 or shunt formation, which is a short, low-resistance, and high-flow pathway12, 13.Conclusion
BAT, a quantitative UF-DCE DISCO parameter, may be a complementary parameter to conventional steady-state DCE MRI, which could further stratify subcentimeter BI-RADS 4 and 5 lesions potentially improving the positive predictive value and ultimately decreasing the number of biopsy recommendations.Acknowledgements
We thank Ms. Maggie Fung, GE Healthcare for her technical support for GenIQ.
This work was supported by NCI P30 Cancer Center Support Grant (CCSG) (P30 CA008748)
References
1. Pineda FD, Medved M, Wang S, Fan X, Schacht DV, Sennett C, et al. Ultrafast Bilateral DCE-MRI of the Breast with Conventional Fourier Sampling: Preliminary Evaluation of Semi-quantitative Analysis. Acad Radiol. 2016 Sep;23(9):1137–44.
2. Mann RM, Mus RD, van Zelst J, Geppert C, Karssemeijer N, Platel B. A novel approach to contrast-enhanced breast magnetic resonance imaging for screening: high-resolution ultrafast dynamic imaging. Invest Radiol. 2014 Sep;49(9):579–85.
3. Mus RD, Borelli C, Bult P, Weiland E, Karssemeijer N, Barentsz JO, et al. Time to enhancement derived from ultrafast breast MRI as a novel parameter to discriminate benign from malignant breast lesions. Eur J Radiol. 2017 Apr;89:90–6.
4. Abe H, Mori N, Tsuchiya K, Schacht DV, Pineda FD, Jiang Y, et al. Kinetic Analysis of Benign and Malignant Breast Lesions With Ultrafast Dynamic Contrast-Enhanced MRI: Comparison With Standard Kinetic Assessment. AJR Am J Roentgenol. 2016 Nov;207(5):1159–66.
5. Cheng Z, Wu Z, Shi G, Yi Z, Xie M, Zeng W, et al. Discrimination between benign and malignant breast lesions using volumetric quantitative dynamic contrast-enhanced MR imaging. Eur Radiol. 2017 Sep 19;
6. Chhor CM, Mercado CL. Abbreviated MRI protocols: wave of the future for breast cancer screening. AJR Am J Roentgenol. 2017 Feb;208(2):284–9.
7. Meissnitzer M, Dershaw DD, Feigin K, Bernard-Davila B, Barra F, Morris EA. MRI appearance of invasive subcentimetre breast carcinoma: benign characteristics are common. Br J Radiol. 2017 Jun;90(1074):20170102.
8. Ha R, Sung J, Lee C, Comstock C, Wynn R, Morris E. Characteristics and outcome of enhancing foci followed on breast MRI with management implications. Clin Radiol. 2014 Jul;69(7):715–20.
9. Liberman L, Mason G, Morris EA, Dershaw DD. Does size matter? Positive predictive value of MRI-detected breast lesions as a function of lesion size. AJR Am J Roentgenol. 2006 Feb;186(2):426–30.
10. Pries AR, Höpfner M, le Noble F, Dewhirst MW, Secomb TW. The shunt problem: control of functional shunting in normal and tumour vasculature. Nat Rev Cancer. 2010 Aug;10(8):587–93.
11. Jain RK, Martin JD, Stylianopoulos T. The role of mechanical forces in tumor growth and therapy. Annu Rev Biomed Eng. 2014 Jul 11;16:321–46.
12. Kul S, Cansu A, Alhan E, Dinc H, Reis A, Çan G. Contrast-enhanced MR angiography of the breast: Evaluation of ipsilateral increased vascularity and adjacent vessel sign in the characterization of breast lesions. AJR Am J Roentgenol. 2010 Nov;195(5):1250–4.
13. Schmitz AC, Peters NHGM, Veldhuis WB, Gallardo AMF, van Diest PJ, Stapper G, et al. Contrast-enhanced 3.0-T breast MRI for characterization of breast lesions: increased specificity by using vascular maps. Eur Radiol. 2008 Feb;18(2):355–64.
Figures
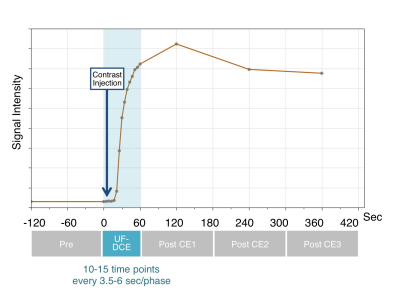
Figure 1: Scan Timing of Ultrafast Dynamic Contrast Enhanced (UF-DCE) MRI Using DISCO
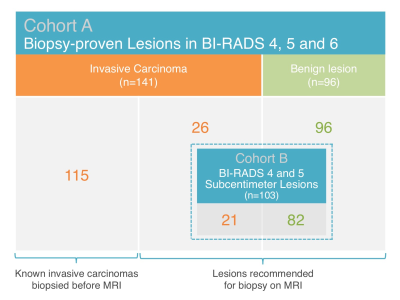
Figure 2: Lesion Characteristics
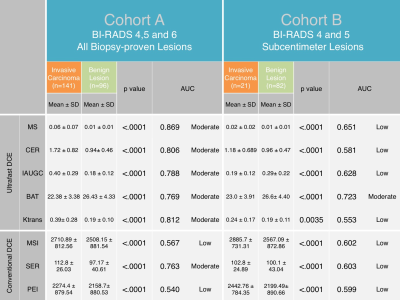
Figure 3: Quantitative Parameters: Comparison between Invasive Carcinomas and Benign Lesions and Diagnostic Accuracy to Predict Invasive Carcinoma
MS, Maximum slope; CER, contrast enhancement ratio; IAUGC, initial area under the gadolinium curve; BAT, bolus arrival time; SER, signal enhancement ratio; MSI, Maximum slope of increase; PEI, positive enhancement integral