0097
ACRIN 6702 Multisite Breast DWI Trial: Comparison of Site vs. Centralized ADC Measures and Factors Affecting Data Quality1Radiology, University of Washington, Seattle, WA, United States, 2ACRIN Biostatistics Center, Brown University, Providence, RI, United States, 3Hematology/Oncology, Vanderbilt University, Nashville, TN, United States, 4Biomedical Engineering, University of Texas, Austin, TX, United States, 5Radiology, University of Michigan, Ann Arbor, MI, United States
Synopsis
Diffusion-weighted imaging (DWI) shows potential to improve lesion characterization and diagnostic performance of conventional contrast-enhanced breast MRI. Promising preliminary data from the ACRIN 6702 multisite trial show that DWI can reduce false-positive breast MRIs. Comparison of independently performed site and centrally-measured ADC values showed reasonable agreement, but suggest that further standardization of DWI interpretation and analysis tools across sites could improve diagnostic performance. Results also show more work is needed to address image quality issues and increase utility for measuring ADC values in MRI-detected breast lesions.
Purpose
Breast MRI is highly sensitive for breast cancer detection and increasingly used for high risk screening and other applications, but moderate specificity results in many unnecessary biopsies [1]. Diffusion-weighted imaging (DWI) has demonstrated promise in numerous single center studies to help reduce the false positive rate of conventional breast MRI [2]. However, variable acquisition and analysis approaches across studies limit ability to establish generalizable guidelines for integration of DWI into routine clinical breast MRI assessments. Towards this goal, the American College of Radiology Imaging Network (ACRIN) 6702 trial investigated DWI performance for diagnosing breast lesions using a standardized protocol in a multisite, multiplatform setting [3]. Encouraging initial results from the trial demonstrated that use of an apparent diffusion coefficient (ADC) threshold could reduce unnecessary biopsies by 21% without reducing sensitivity [4]. As a secondary aim, we sought to determine whether site-generated ADC values differed significantly from those obtained by central review, and to assess factors affecting data quality.Materials and Methods
The IRB-approved trial was performed at ten institutions on multiple 1.5T and 3T MRI platforms (Philips, GE, and Siemens) from March 2014 to April 2015. All participants provided informed consent prior to undergoing clinical breast MRI, and a standardized DWI sequence was performed during their exams. Women with dynamic contrast-enhanced (DCE)-MRI-detected BI-RADS 3, 4, or 5 lesions were enrolled in the study. DWI was acquired prior to DCE-MRI using a single shot diffusion-weighted spin-echo echo planar imaging (EPI) sequence with parallel imaging, fat suppression, and b-values = 0, 100, 600, and 800 s/mm2. Reference standard for lesion outcome was biopsy or one year negative clinical/imaging follow-up. Lesion ADC values were measured prospectively by the sites using varying available software tools, and retrospectively by the centralized core facility, with investigators blinded to lesion outcomes. Centralized lesion ROIs were defined independent of site ROIs, with lesions identified based on imaging reports and DCE images. During centralized analysis, each DWI scan was first reviewed for image quality factors: fat suppression, signal-to-noise ratio (SNR), artifacts, and misregistration. Lesions were considered not evaluable if significant image quality factors and/or lack of lesion visibility prevented ADC measurement. ADC values of malignant and benign lesions were compared by bootstrap. Site-generated and centrally-measured lesion ADC values were compared by bootstrap method, and diagnostic performance for differentiating benign and malignant lesions was assessed by Receiver Operator Characteristic (ROC) curve analyses.Results
ACRIN 6702 included 103 women (with 142 lesions) who completed the study, of which 28 lesions in 21 women were missing the reference standard to determine benign/malignant outcome. Of 103 MRI examinations, 42 (41%) were performed at 1.5T and 61 (59%) at 3T.
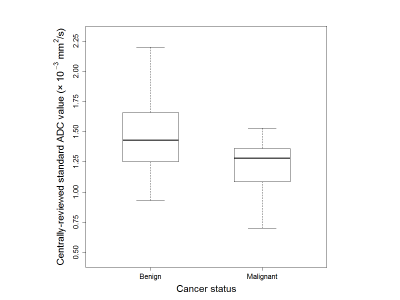
Centralized DWI analysis: Of the 114 lesions with reference standard (34 malignant, 80 benign), image quality was deemed low and/or ADC not-evaluable in 33/114 (28.9%) lesions. Factors observed to be most associated with non-evaluability included misregistration, small lesion size (<10mm), and benign histology, but not lesion type (mass vs. non-mass) or magnetic field strength. In the 81 evaluable lesions (28 malignant, 53 benign), malignancies exhibited lower central ADC than benign lesions (1.21 ±0.21 vs. 1.47 ±0.29 ×10-3 mm2/s, p<0.0001, Figure 1); the area under the ROC curve (AUC) for predicting malignancy was 0.75 (95% CI=0.65-0.85).
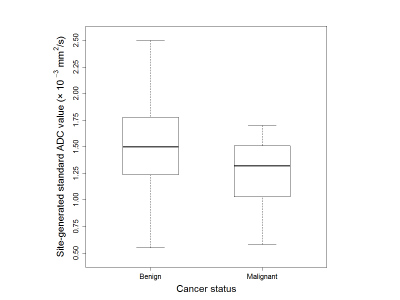
Site ADC measures: Site-generated ADCs were submitted for 70/81 evaluable lesions (26 malignant, 44 benign). Site ADC was significantly lower in malignancies versus benign lesions (1.30 ± 0.43 vs. 1.52 ± 0.42 ×10-3 mm2/s, p=0.0375, Figure 2), and AUC for predicting malignancy was 0.66 (95% CI=0.53-0.78).
Site vs. central ADC measures: In the 70 evaluable lesions where both site and central ADC were available, site-generated ADCs were slightly higher than centrally-reviewed ADCs on average (1.44 ×10-3 vs. 1.37 ×10-3 mm2/s), but did not reach statistical significance (p=0.064). There was a trend for higher performance in predicting malignancy using central versus site ADC measures, although the difference was not significant (AUC=0.76 vs. 0.66, p=0.069), Figure 3.
Conclusion
ACRIN 6702 multisite breast DWI trial results showed independent site and centralized lesion ADC measures agreed relatively well despite varying approaches. Differences in diagnostic performance of site and centralized ADC measures suggest need to further standardize DWI interpretation and analysis tools across sites. Additionally, image quality remains a challenge for clinical implementation of breast DWI, with ADC not measurable in 30% of lesions. Further optimizations and technical advancements to improve the image quality of breast DWI imaging protocols are needed to facilitate the clinical translation of DWI to reduce breast MRI false-positives.Acknowledgements
This research was supported by the American College of Radiology Imaging Network, ACRIN, which receives funding from the National Cancer Institute (NCI) through the grants U01 CA079778 and U01 CA080098. Performance of central DWI analysis was supported by NIH/NCI R01CA151326.References
1. Peters NH, Borel Rinkes IH, Zuithoff NP, Mali WP, Moons KG, Peeters PH. Meta-analysis of MR imaging in the diagnosis of breast lesions. Radiology. 2008;246(1):116-24.
2. Zhang L, Tang M, Min Z, Lu J, Lei X, Zhang X. Accuracy of combined dynamic contrast-enhanced magnetic resonance imaging and diffusion-weighted imaging for breast cancer detection: a meta-analysis. Acta Radiol. 2016;57(6):651-60.
3. ACRIN 6702: A Multi-Center Study Evaluating the Utility of Diffusion Weighted Imaging for Detection and Diagnosis of Breast Cancer. https://clinicaltrials.gov/ct2/show/NCT02022579.
4. Partridge SC, Zhang Z, Rahbar H, Chenevert TL, Kitsch AE, Hanna L, Romanoff J, Harvey S, Moy L, DeMartini W, Schnall M, Lehman CD, Comstock C. ACRIN 6702 Trial: A Multicenter Study Evaluating the Utility of Diffusion Weighted Imaging for Detection and Diagnosis of Breast Cancer. Accepted for presentation at RSNA, Chicago, IL, Nov 2017.
Figures