0066
Arterial-Spin-Labeling (ASL) perfusion MRI predicts cognitive function in elderly individuals: a four-year longitudinal study1MR Research, Johns Hopkins University, Baltimore, MD, United States, 2Biomedical Imaging and Radiological Science, China Medical University, Taichung, Taiwan, 3Center for Vital Longevity, School of Behavioral and Brain Sciences, University of Texas, Dallas, TX, United States
Synopsis
Identification of biomarkers that can predict cognitive decline is of utmost importance for advance in dementia pharmacotherapy. In this study, cerebral blood flow (CBF) is investigated as a predictor for cognitive decline in a healthy aging population. We found CBF in the frontal lobe to be most predictive for cognitive decline, specifically for episodic memory and in the older population. This suggest that CBF can be used as a biomarker to identify subjects susceptible to cognitive decline, to identify suitable cohorts for clinical trials, and to monitor the effects of pharmacotherapy.
Introduction
With the disappointing outcomes of clinical trials on patients with Alzheimer’s disease or Mild-Cognitive-Impairment (MCI)1, there is increasing attention to understanding cognitive decline in normal elderly individuals, with the goal of identifying subjects who are most susceptible to imminent cognitive impairment. Brain structural and functional changes are known to coincide with age-related cognitive decline2-4. However, the association between neurobiological changes and cognition is poorly understood. In this study, we investigated the potential of Cerebral Blood Flow (CBF) in predicting cognitive performance in a longitudinal setting.Methods
Three hundred and nine subjects were recruited from a longitudinal life span study on cognitive aging and neuroimaging. Inclusion criteria of the study were; (1) age 20-89 years, (2) mini-mental state exam (MMSE) > 26, (3) good health, and (4) no contra-indications for MRI. Data was gathered at two-time points with a mean interval of 4.1 (±0.2) years between both time points.
Magnetic resonance imaging was performed at visit 1 and at a 3T Philips scanner, it consisted of a T1-weighted magnetization-prepared rapid acquisition of gradient echo (T1-MPRAGE) and a pseudocontinuous Arterial Spin Labeling (pCASL) sequence. The scan parameters of the T1-MPRAGE sequence were; TR/TE/TI = 8.1 ms/3.7 ms/1100 ms, voxel size 1x1x1 mm3 and duration 3 min and 57s. Scan parameters of the pCASL sequence were; TR/TE = 4020 ms/14 ms, voxel size 3x3x5 mm3, labeling duration = 1.65s, post-labeling delay = 1.5 s, single-shot echo-planar imaging (EPI), 30 pairs of label and control images, and duration 4 min. T1-multi-atlas and ASL toolboxes of MRICloud were used for MRI data analysis5,6. Whole-brain gray matter and lobar gray matter CBF (frontal, parietal, temporal, and occipital) were evaluated.
Four domains of cognitive function were assessed at visit 1 and 2: processing speed, working memory, reasoning, and episodic memory. A composite fluid ability score was obtained by averaging these domain scores.
The relation between CBF at visit 1 and cognition at visit 2 was investigated using linear regression analyses correcting for age and cardiovascular indices of health (blood pressure and physical activity), as these have a known association with cognition2,7,8.
Results
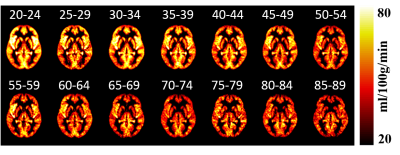
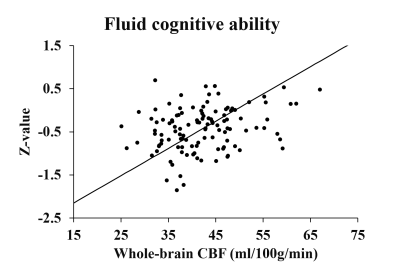
Of the 309 subjects, 10 subjects were excluded due to poor pCASL image quality (N=10). The mean age of the remaining 299 subjects was 54(±20) years, and there was a significant age-related decrease in CBF and fluid ability within this group (p<0.001, Figure 1 and 2).
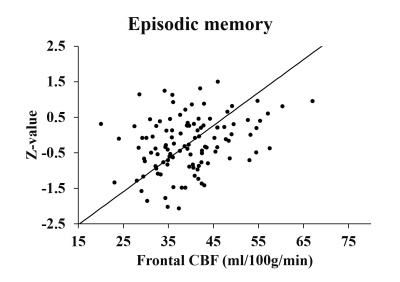
Of the 299 subjects, 216 subjects returned for visit 2 which restricted our longitudinal analysis to this number. Whole-brain and frontal CBF at visit 1 were associated with fluid ability at visit 2 (β=0.221, p=0.004 and β=0.244, p=0.001, Figure 3) in older individuals (age ≥ 54yrs). For frontal CBF, this effect was also observed in the entire population (β=0.116, p=0.031). Furthermore, frontal CBF at visit 1 and fluid ability at visit 2 remain associated (p=0.049) after accounting for fluid ability at visit 1. The cognitive domain with which frontal CBF had the strongest relationship was episodic memory and this relationship was observed in the older group (β=0.294, p=0.001, Figure 4) and in the entire cohort (β=0.205, p=0.006). Frontal CBF also showed a predictive value for reasoning ability in the older group (β=0.186, p=0.027).
An association was also found between parietal CBF at visit 1 and processing speed at visit 2 in the older group (β=0.179, p=0.017). Parietal CBF was also associated with change in reasoning between visit 1 and 2 (β=0.209, p=0.029 in the older group and β=0.018, p=0.018 in the entire cohort).
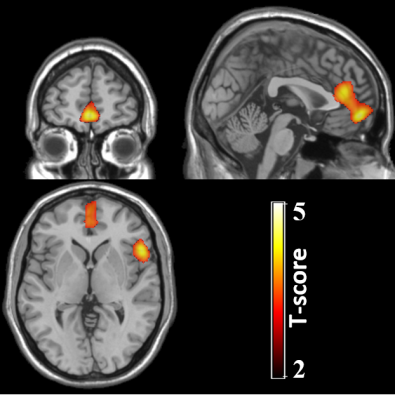
A voxel-wise analysis performed to corroborate the lobar results found significant clusters in the frontal lobe, in particular in the medial frontal cortex and anterior cingulate cortex (ACC), which were related to visit 2 fluid ability in the older cohort (Figure 5).
Discussion
Data of this longitudinal aging study demonstrate that non-invasive CBF imaging can predict cognition in healthy aging. Frontal lobe CBF is the most sensitive in predicting future cognition, especially in the cognitive domain of episodic memory. CBF in the medial frontal cortex/anterior cingulate cortex seems particularly important for an individual’s cognitive ability. Our findings suggest that imaging measures of brain perfusion may provide a useful biomarker for early detection of cognitive decline, identification of suitable cohorts for clinical trials, and monitoring of treatment effects.Conclusion
Cerebral blood flow measured with non-invasive MRI can predict cognitive scores four year later. In particular, cerebral blood flow in the frontal lobe is strongly predictive of episodic memory.Acknowledgements
No acknowledgement found.References
1. Sperling RA, Jack CR, Aisen PS. Testing the Right Target and Right Drug at the Right Stage. Sci Transl Med. 2011;3(111):111cm33.
2. Park DC, Nisbett R, Hedden T. Aging, culture, and cognition. J Gerontol B Psychol Sci Soc Sci. 1999;54(2):75-84.
3. Fjell AM, Westlye LT, Grydeland H, et al. Accelerating Cortical Thinning: Unique to Dementia or Universal in Aging? Cereb Cortex. 2014;24(4):919-934.
4. Rieck JR, Rodrigue KM, Boylan MA, et al. Age-related reduction of BOLD modulation to cognitive difficulty predicts poorer task accuracy and poorer fluid reasoning ability. Neuroimage. 2017;147:262-271.
5. Mori S, Wu D, Ceritoglu, et al. MRICloud: Delivering high-throughput MRI neuroinformatics as cloud-based software as a service. Comput Sci Eng. 2016;18:21-35.
6. Li Y, Liu P, Fan H, et al. ASL-MRICloud: Towards a comprehensive online tool for ASL data analysis. Int Soc Magn Reson Med Annual Meeting. 2017:3808.
7. Fratiglioni L, Paillard-Borg S, Winblad B. An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurol. 2004;3(6):343-353.
8. Hughes TM, Sink KM. Hypertension and Its Role in Cognitive Function: Current Evidence and Challenges for the Future. Am J Hypertens. 2016;29(2):149-157.
Figures