0015
4D Flow Cardiac MRI Using Semi-Automated Retrospective Valve Tracking for Assessment of Severe Mitral Insufficiency1Academic Medical Center Amsterdam, Amsterdam, Netherlands, 2Leiden University Medical Center, Leiden, Netherlands, 3Utrecht University Medical Center, Utrecht, Netherlands, 4Pie Medical Imaging, Maastricht, Netherlands
Synopsis
Mitral insufficiency (MI) is difficult to quantify, due to cardiac motion and complex regurgitation patterns. This study evaluated the use of 4D flow MRI with semi-automated retrospective valve tracking for assessment of severe MI. Valve tracking of both the mitral and aortic valve allowed for direct measurement of retrograde flow and indirect measurement based on total left-ventricular inflow and aortic outflow. Conventional 2D MRI-based indirect quantification was used as a reference. Eccentric regurgitation patterns complicated direct quantification, necessitating manual plane angulation for accurate measurement. Indirect quantification corresponded well with 2D MRI and might be a more reproducible alternative.
Introduction
Mitral insufficiency (MI, or mitral regurgitation) is a common valvular heart defect which is clinically quantified with 2-dimensional (2D) Doppler echocardiography. However, this technique is limited by geometrical assumptions and operator dependency. Quantification by cardiac 2D MRI is more reproducible, but has to be performed in an indirect manner based on left-ventricular (LV) stroke volume and aortic flow, since 2D phase-contrast (PC) MRI over the mitral valve does not optimally account for annular motion and the valve’s complex anatomy. Cardiac 4D flow MRI with retrospective valve tracking offers novel possibilities to quantify transvalvular blood flow with good correlation across heart valves.1,2 Its application to severe MI was never studied before. We aimed to evaluate the accuracy of 4D flow MRI using semi-automated retrospective valve tracking for assessment of severe MI in a comparison with an indirect 2D MRI-based approach.Methods
10 patients (80% male, mean age 59±10y) with asymptomatic severe MI as diagnosed by echocardiography according to ESC guidelines3 and without other valvular disease underwent cardiac MRI including 4D flow MRI at 1.5T. 4D flow was acquired in 30 cardiac phases during free-breathing with retrospective ECG-gating. Reconstructed spatial resolution was 2.89x2.89x3.5mm, temporal resolution was 27-37ms and three-directional VENC was set to 180 cm/s. Retrospective tracking of the mitral valve (MV) and aortic valve (AV) was performed using 2D cine bSSFP by dedicated software (CAAS MR 4D Flow 2v0, Pie Medical Imaging) with through-plane valve motion correction and automatic aliasing and phase offset correction. For the MV, an additional analysis was performed with the quantification plane angulated perpendicular to the regurgitation jet, and positioned approximately 1 cm above the valve. Time-resolved streamlines were generated for visual verification. 2D flow measurements at the level of the AV were performed using a 2D PC-MRI acquisition in 20 cardiac phases. LV stroke volume was determined by means of short-axis bSSFP planimetry.
4D flow-derived LV inflow and outflow were calculated as summations of MV and AV antegrade and retrograde flows. MV regurgitant volume (Rvol) was calculated using 4D flow data by assessment of a) regurgitant MV flow and b) LV inflow minus antegrade AV flow. Furthermore, Rvol was derived from 2D MRI data by subtracting antegrade AV flow from LV stroke volume. Rvol was divided by either LV inflow (4D flow) or stroke volume (2D MRI) to obtain regurgitation fraction. Agreements and differences were assessed with Pearson’s correlation test (R- and P-value) and Student’s t test (p-value) respectively. P<0.05 was considered significant.
Results
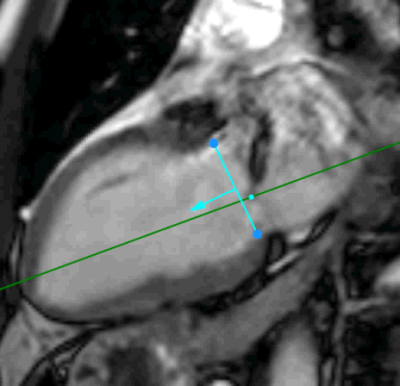
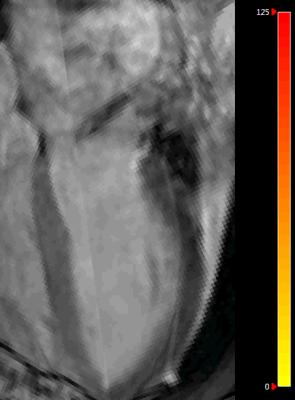
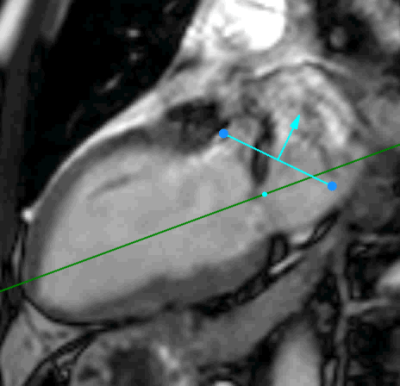
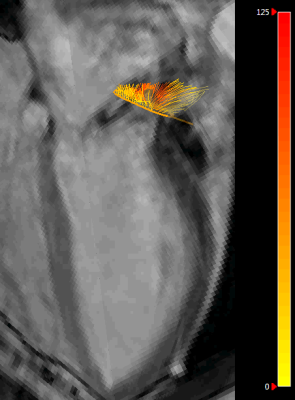
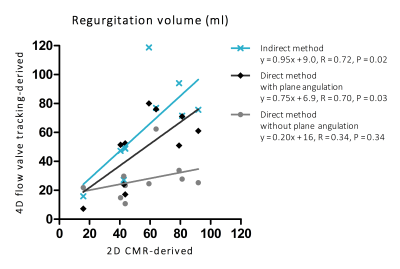
Highly eccentric and complex regurgitation patterns were observed. For a demonstration of how valve tracking with plane angulation was performed in a patient with eccentric regurgitation, see Figure 1 and Figure 2 for antegrade flow and Figure 3 and Figure 4 for retrograde flow. 4D flow-derived Rvol by direct quantification (without plane angulation) of retrograde MV flow (27±14ml) was lower than 2D MRI-derived Rvol (56±23ml) (R=0.34, P=0.34, p=0.004). Rvol after plane angulation (49±25ml) showed no difference with 2D MRI (R=0.70, P=0.03, p=0.52), as well as 4D flow-derived Rvol by indirect quantification based on LV inflow and AV antegrade flow (62±31ml) (R=0.72, P=0.02, p=0.61); Figure 5. With the latter method, regurgitation fractions of 39±13% were found. 4D flow-derived LV inflow (154±37ml) did not differ from LV stroke volume based on bSSFP planimetry (152±30ml) (p=0.85), and antegrade AV flow by 4D flow (92±21ml) corresponded well with 2D-PC measurement (96±19ml) (p=0.70).Discussion
In this study we applied 4D flow MRI with retrospective valve tracking in patients with severe MI. Eccentricity of regurgitation patterns gave rise to underestimation of retrograde flow when valve tracking was performed without angulation with respect to the jet’s direction. This finding can be explained by the fact that only through-plane velocities were taken into account in the flow calculation. When jet angulation was adjusted for and the quantification plane was shifted up into the left atrium, direct quantification of Rvol using 4D flow MRI and retrospective valve tracking agreed better with the 2D MRI-based approach. Indirect 4D flow-derived quantification combining mitral and aortic flow corresponded best with 2D MRI and might be a quicker and more reproducible alternative, as it requires less manual intervention in the valve tracking process. Future work should involve a larger cohort and multiple observers to investigate which quantification method is most appropriate for assessment of severe MI.Conclusion
Eccentric regurgitation patterns complicate direct quantification of retrograde flow by means of retrospective valve tracking in patients with severe and complex MI. Indirect 4D flow-derived quantification might be more accurate and could eventually replace currently performed, but time-inefficient, 2D MRI-based quantification.Acknowledgements
No acknowledgement found.References
1. Roes, S. D. et al. Flow assessment through four heart valves simultaneously using 3-dimensional 3-directional velocity-encoded magnetic resonance imaging with retrospective valve tracking in healthy volunteers and patients with valvular regurgitation. Invest. Radiol. 44, 669–75 (2009).
2. Hsiao, A., Tariq, U., Alley, M. T., Lustig, M. & Vasanawala, S. S. Inlet and outlet valve flow and regurgitant volume may be directly and reliably quantified with accelerated, volumetric phase-contrast MRI. J. Magn. Reson. Imaging 41, 376–385 (2015).
3. Vahanian,
A. et al. [Guidelines on the management of valvular heart disease
(version 2012). The Joint Task Force on the Management of Valvular Heart
Disease of the European Society of Cardiology (ESC) and the European Association
for Cardio-Thoracic Surgery (EACTS)]. G. Ital. Cardiol. (Rome). 14,
167–214 (2013).
Figures