0008
Quantifying the Impact of Velocity Field Distortions on Particle Tracking Techniques1Linköping University, Linköping, Sweden, 2Center for Medical Image Science and Visualization (CMIV), Linköping, Sweden, 3University Hospital Linköping, Linköping, Sweden
Synopsis
Distortions in the velocity fields acquired by 4D Flow MRI affect particle tracking based visualization and quantification methods. Particle residence time was calculated in a subject with aortic aneurysm and was used to assess how particle tracking methods are impacted by noise and offset errors. To do so, a computationally derived ideal velocity field was created and distorted by adding noise and background phase-offsets. We found that particle tracking methods are severely impacted by offset errors, though more robust to random noise. Understanding the limits of these methods is crucial for their appropriate use.
Introduction
4D Flow MRI data is complex, and a variety of techniques are used for visualization and quantification. One popular approach is particle tracking(PT), where virtual particles are released and their movements are followed through time. This method is popular for visualization (1) and to a growing extent quantification (2–4). Unfortunately, 4D Flow MRI data is affected by distortions such as noise and background phase-offsets(‘Offsets’)(1,5). Noise causes random errors in the velocity field, while offsets cause non-random bias fields that can create the appearance of non-physiological flow patterns. Therefore, the aim of this study was to examine the effects of these typical distortions to the acquired 4D Flow MRI velocity fields on PT methods. To do so, we quantified the effects of these distortions on particle residence time calculations using an ideal velocity field for a subject with infra-renal abdominal aortic aneurysm (AAA) generated using computational fluid dynamics (CFD). This synthetic 4D Flow data served as a platform to which distortions could be applied and the effects of errors could be analysed.Methods
The sensitivity of PT to noise and offset errors was analyzed by gradually degrading ideal synthetic velocity data, obtained using CFD. The CFD simulation was performed using ANSYS CFX 17.0 (ANSYS Inc., Canonsburg, PA). AAA geometry and flow profiles used for boundary conditions were derived from contrast-enhanced MR angiography (CE-MRA) and 4D Flow data, respectively. The CE-MRA was acquired with a spatial resolution of 0.6 x 0.6 x 1.2 mm and the 4D Flow data was acquired using a free-breathing, respiratory and cardiac-gated sequence with 2.5 mm isotropic spatial resolution and 35 ms temporal resolution, following the CE-MRA. All data was acquired using a 3T scanner (Philips Ingenia, Philips Healthcare). Synthetic 4D Flow data was created by sampling the ideal CFD velocity field with a kernel representing the spatial and temporal characteristics of 4D Flow voxels.
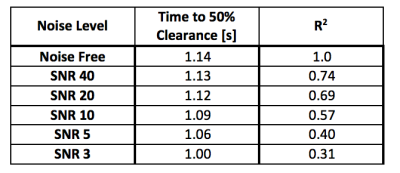
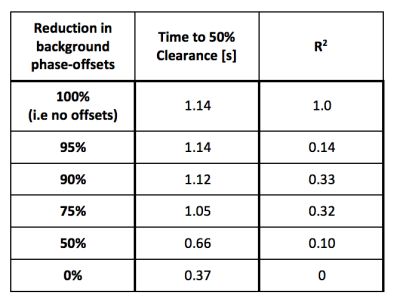
Five levels of noise were added to the synthetic 4D Flow data, corresponding to signal-to-noise ratio (SNR) levels of: 3, 5, 10, 20, and 40. Offsets derived from the 4D Flow correction for this patient were approximately 1.5 cm/s on average, in each direction, inside the AAA. Offset correction was performed using a 4th order fit to static tissue(6). The offsets’ impact was examined by progressively reducing their strength. Five levels were examined, corresponding to reductions in the offsets of: 0% (i.e., no reduction), 50%, 75%, 90%, and 95%.
Residence Time was calculated using the ideal and distorted data by releasing particles from the centre of every voxel within the AAA and tracing their movements forward 10 cycles. The total accumulated time that particles spent in each voxel was measured, alongside the time until 50% of the particles had exited the volume of interest (’50% clearance time’). Residence time results were compared using linear regression against results from the ideal data.
Results
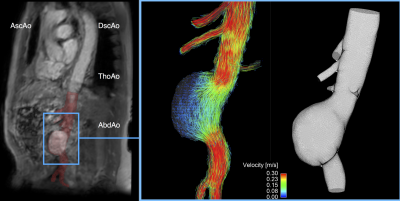
An overview of the patient anatomy used for assessing PT is seen in Figure 1. This subject with a large saccular AAA exhibits large recirculating vortices in the aneurysmal sac and areas of low flow velocity.
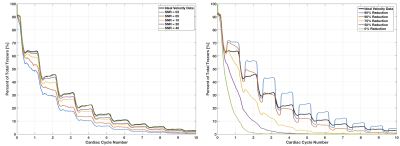
Noise affected the quality of PT, as assessed through the calculation of residence time (Table 1). At SNR = 20, typical to 4D Flow MRI, there is a substantial impact, with R2 = 0.68, though only a small reduction in 50% clearance time.
The presence of offsets similarly impacted residence time results (Table 2). Considering a velocity field with offsets at full impact, no correlation was found between residence time results to those derived from the ideal data. The time until 50% particle clearance was also drastically reduced. Offsets altered the flow pattern, and caused particles to exit the aneurysm through the vascular wall.
The particle washout profile shows the altered flow pattern caused by poorer quality PT in aggregate by showing the proportion of particles inside the aneurysm through time (Figure 2). Comparing washout profiles against the ideal case demonstrates the aggregate impact to PT caused by poor data quality.
Discussion
4D Flow MRI Data is affected by distortions that impact visualizations and quantifications using PT methods. Noise is damaging to quantification methods, though at SNR levels common to 4D Flow MRI the affect is moderate if the traces are kept relatively short. Offsets are particularly damaging to PT methods, as they can generate unrealistic flow patterns which dramatically alter the results. Therefore, as demonstrated here for the application of measuring particle residence time in aneurysms, investigating the effects of common 4D Flow artifacts on PT is critical to understanding the limits of these methods.Acknowledgements
No acknowledgement found.References
1. Dyverfeldt P, Bissell M, Barker AJ, et al. 4D flow cardiovascular magnetic resonance consensus statement. J. Cardiovasc. Magn. Reson.2015;17:72. doi: 10.1186/s12968-015-0174-5.
2. Eriksson J, Carlhäll C, Dyverfeldt P, Engvall J, Bolger AF, Ebbers T. Semi-automatic quantification of 4D left ventricular blood flow. J. Cardiovasc. Magn. Reson.2010;12:9. doi: 10.1186/1532-429X-12-9.
3. Fredriksson AG, Zajac J, Eriksson J, Dyverfeldt P, Bolger AF, Ebbers T, Carlhäll C-J. 4-D blood flow in the human right ventricle. Am. J. Physiol. Heart Circ. Physiol.2011;301:H2344-50. doi: 10.1152/ajpheart.00622.2011.
4. Callaghan FM, Grieve SM. Spatial resolution and velocity field improvement of 4D-flow MRI. Magn. Reson. Med.2016. doi: 10.1002/mrm.26557.
5. Busch J, Giese D, Kozerke S. Image-based background phase error correction in 4D flow MRI revisited. J. Magn. Reson. Imaging 2017. doi: 10.1002/jmri.25668.
6. Ebbers T, Haraldsson H, Dyverfeldt P, Sigfridsson A, Warntjes MJB, Wigström L. Higher order weighted least-squares phase offset correction for improved accuracy in phase-contrast MRI. In: 16th meeting of the International Society for Magnetic Resonance in Medicine. Toronto; 2008. p. 1367.
Figures