MR Imaging Around Metal: Clinical Applications
1Radiology faculty, Stanford University Medical Center, Stanford, CA, United States
Synopsis
Metal implants are now commonplace in modern medicine. MRI evaluation of symptomatic patients with orthopedic hardware used to be severely limited by susceptibility artifact. However, recent advances in metal suppression techniques allow improved imaging around metal, making MRI effective for evaluation of patients with symptomatic implants, even at higher magnetic field strengths. This lecture will cover some of the common clinical applications of metal suppression MRI, particularly with respect to total hip and knee arthroplasties, and will also demonstrate the utility of metal suppression with respect to other implants and in the evaluation of patients with spinal hardware.
Highlights
· MR imaging of patients with metal implants at higher magnetic fields strengths is now possible using metal artifact reduction sequences (MARS)
· Total hip arthroplasties are associated with a variety of complications depending on their composition and many of these can be readily seen on MRI
· The utility of MRI will be illustrated in a variety of other implants including total knee arthroplasties and spinal implants
Objectives
· Review different types of total hip arthroplasty
· Describe and classify complications arising from total hip arthroplasty on MRI
· Outline complications occurring with other total joint replacements
· Illustrate the utility of metal suppression MRI in imaging patients with spinal hardware and other metallic implants
Introduction
Total joint arthroplasties are effective in the treatment of end stage osteoarthritis and can be effective in relieving joint pain and improving function. The number of total hip and total knee arthroplasties being performed has increased dramatically in recent years, and are increasingly being performed in younger and more physically active individuals. Arthroplasties have a limited life span despite improvements in arthroplasty design and fixation techniques, which will lead to increased demand for revision arthroplasties in the future. Arthroplasties are routinely monitored using plain radiographs, but these can be insensitive in the detection of early hardware complications. Magnetic resonance imaging with metal reduction techniques has emerged as the imaging modality of choice for the evaluation of osseous and soft tissue complications that may be occult radiographically, and is now used routinely in the work up of patients being considered for revision arthroplasty.
Choice of implant
A variety of different materials have been used in total joint arthroplasties in efforts to increase longevity of the implant. Metal-on-polyethylene (MoP) implants are one of the most popular choices, comprising a cobalt-chrome metal alloy articulating with a polyethylene liner or polyethylene acetabular component. However, the polyethylene component tends to wear out over time, particularly with younger active patients, resulting in particle disease, bone loss and loosening. Highly cross-linked ultra-high molecular weight polyethylene is more durable, but still subject to wear. Alternative materials, head sizes and fixation techniques have been developed in efforts to minimize wear, decrease complications and improve patient outcomes, including metal-on-metal (MoM) prostheses, ceramic-on-polyethylene (CoP) and ceramic-on-ceramic (CoC) components. Metal-on-metal arthroplasties were initially favored for younger patients due to the low rate of wear, but a high overall failure rate was reported. Wear of the metal-on-metal implants results in the production of microscopic metallic debris which can distribute in the adjacent soft tissues, triggering either a foreign body-type reaction or lymphocyte-mediated delayed hypersensitivity-type reaction, both resulting in injury to the periprosthetic tissues. Metal ions may also distribute systemically, leading to fatigue, muscle weakness and cramps, tremor, hypothyroidism, polycythemia, depression, cognitive dysfunction, hearing loss, neuropathy, and even fatal cardiomyopathy and arrhythmias. More recently hip arthroplasties with modular components have been introduced, giving the orthopaedic surgeon the option to adjust for leg length and hip offset. However, these modular components have also been associated with similar adverse local tissue reactions due to fretting and corrosion at the modular junctions, particular when modular components are composed of differing metals. Ceramic components made of aluminum oxide and zirconium oxide are both hard and durable, with minimal resultant wear, and are therefore a reasonable choice for younger active patients. Original ceramic implants were associated with catastrophic shattering and “squeaking”, although improvements in implant design have overcome some of these issues. Ceramic prostheses are expensive, but are associated with a low incidence of complications.Complications of total joint arthroplasties
Complications arising from total joint arthroplasties include the following:
· Periprosthetic fracture – intraoperative or secondary to bone resorption, osteolysis, and implant loosening or incorrect implant alignment, often with superimposed trauma. Although many fractures can be seen radiographically, non-displaced periprosthetic fractures or stress reactions can now be seen on MRI.
· Bone resorption and loosening – manifest as increased signal at bone-implant interface measuring greater than 2mm in thickness surrounded by a thin layer of low signal corresponding to a fibrous membrane
· Heterotopic ossification – occurs within 8 weeks of surgery and can develop pain, swelling and warmth in maturation phase mimicking infection. Risk factors include males, lateral approach to THA, use of cemented components, hypertrophic osteoarthritis, previous history of heterotopic ossification, ankylosing spondylitis and DISH. Immature heterotopic ossification may appear as a heterogeneous mass on MRI, mimicking a hematoma, abscess or soft tissue mass, and may be radiographically occult.
· Malalignment and hardware failure – acetabular component of total hip arthroplasty with abduction angle > 50°or anteversion of > 40°, wrong size of components, fracture or dissociation of components
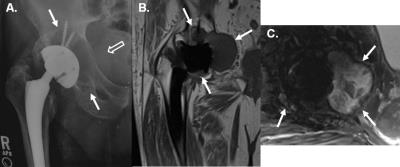
· Particle disease and osteolysis – occurs with polyethylene, methylmethacrylate cement, and metal -triggers histiocytic foreign body reaction with influx of macrophages and release of inflammatory cytokines producing reactive synovitis, activation of osteoclasts and down-regulation of osteoblasts with resultant periprosthetic osteolysis and eventual loosening. Early particle disease can present with a joint effusion and reactive synovitis which may be asymptomatic, or can manifest as low to intermediate signal intensity debris, which may appear solid, with varying amounts of interspersed fluid – a larger burden of disease may decompress into the overlying trochanteric bursa via dehiscence of the posterior pseudocapsule, or anteriorly into the iliopsoas bursa or subiliac bursa. Particle disease may result in periprosthetic osteolysis (Figure 1) and subsequent loosening.
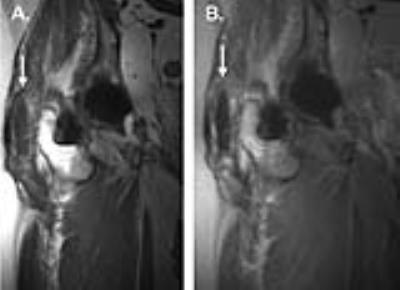
· Adverse reaction to metallic debris (ARMD)- occurs in metal-on-metal prostheses, as well as modular prostheses with fretting (mechanical wear) and/or corrosion at head-neck junction or neck-stem junction and can result in extensive soft tissue necrosis
o Metallosis – shedding of larger metallic debris leads to synovitis with low signal intensity debris – may occur in association with particle disease or metal hypersensitivity
o Particle disease and osteolysis as above, with foci of susceptibility artifact (Figure 2).
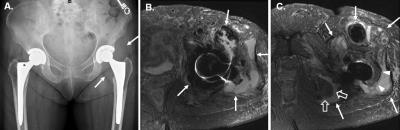
o “Pseudotumor” – type 4 hypersensitivity reaction to metallic ions resulting in Aseptic Lymphocytic Vasculitis-Associated Lesions (ALVAL) manifesting as thin-walled periprosthetic cystic masses, thick-walled cystic masses (Figure 3), or solid masses – all can lead to adjacent soft tissue damage. Increased synovial thickness, size of collection, soft tissue edema, capsular dehiscence and disruption of the gluteal tendons are associated with higher ALVAL scores on histology (Figure 4). However, there is no correction between the histologic severity and serum metal concentrations.
· Infection – enhancing lamellated synovitis, bone marrow edema or destruction, extracapsular edema and enhancement, extracapsular collections and lymphadenopathy.
· Tendon and muscle injury – tendinosis, tendon tears or bursitis from hardware impingement, adverse local tissue reaction, or trauma and muscle atrophy or denervation. Gluteal tendon pathology is common after total hip arthroplasty, and tendons may be disrupted by pseudotumor extension. Impingement of the iliopsoas tendon may occur from a large or incorrectly positioned acetabular cup or large femoral component. Disruption of the extensor mechanism may occur after total knee arthroplasty (Figure 5).
· Nerve injury – may occur intra-operatively, after dislocation of the prosthesis, or from heterotopic ossification, impingement from hardware or adverse local tissue reactions.
Acknowledgements
No acknowledgement found.References
Anderson H, Toms AP, Cahir JG, Goodwin RW, Wimhurst J, Nolan JF. Grading the severity of soft tissue changes associated with metal- on-metal hip replacements: reliability of an MR grading system. Skeletal Radiology 2011; 40(3): 303–7.
Barlow BT, Ortiz PA, Fields KG et al. MRI predicts adverse total tissue reaction histologic severity in modular neck total hip arthroplasty. J Arthroplasty 2016; 10: 2325-2331.
Burge AJ, Gold SL, Lurie B, Nawabi DH, Fields KG, Koff MF, Westrich G, Potter HG. MR imaging of adverse local tissue reactions around Rejuvenate modular dual-taper stems. Radiology 2015; 277(1): 142-150.
Campbell P, Ebramzadeh E, Nelson S, Takamura K, De Smet K, Amstutz HC. Histological features of pseudotumor-like tissues from metal-on-metal hips. Clin Orthop Relat Res. 2010; 468(9): 2321-2327.
Chen CA, Chen W, Goodman SB, Hargreaves BA, Koch KM, Lu W, Brau AC, Draper CE, Delp SL, Gold GE. New MR imaging methods for metallic implants in the knee: artifact correction and clinical impact. J Magn Reson Imaging. 2011 May;33(5):1121-1127.
Choi SJ, Koch KM, Hargreaves BA, Stevens KJ, Gold GE. Metal artifact reduction with MAVRIC SL at 3-T MRI in patients with hip arthroplasty. Am J Roentgenol. 2015; 204(1): 140-147.
Fritz J, Lurie B, Miller TT, Potter HG. MR imaging of hip arthroplasty implants. Radiographics. 2014; 34(4): E106-32.
Fritz J, Lurie B, Potter H. MR imaging of knee arthroplasty implants. RadioGraphics 2015; 35: 1483–1501.
Gutierrez LB, Do BH, Gold GE, Hargreaves BA, Koch KM, Worters PW, Stevens KJ. MR imaging near metallic implants using MAVRIC SL: initial clinical experience at 3T. Acad Radiol. 2015 Mar;22(3):370-9.
Hart AJ, Satchithananda K, Liddle, AD, Sabah SA. McRobbie D, Henckel J, Cobb JP, Skinner JA, Mitchell AW. Pseudotumors in association with well-functioning metal-on-metal hip prostheses: A case control study using 3-dimensional computed tomography and magnetic resonance imaging. JBJS (Am) 2012; 94: 317 – 325.
Hauptfleisch J, Pandit H, Grammatopoulos G, Gill HS, Murray DW, Ostlere S. An MRI classification of periprosthetic soft tissue masses (pseudotumours) associated with metal-on-metal resurfacing hip arthroplasty. Skeletal Radiology 2012; 41(2): 149–155.
Jarrett CA, Ranawat AS, Bruzzone M, Blum YC, Rodriguez JA, Ranawat CS. The squeaking hip: A phenomenon of ceramic-on-ceramic total hip Arthroplasty. J Bone Joint Surg Am. 2009; 91(6): 1344–1349.
Kwon YM, Ostlere SJ, McLardy-Smith P, Athanasou NA, Gill HS, Murray DW. ‘‘Asymptomatic’’ pseudotumors after metal-on-metal hip resurfacing arthroplasty: prevalence and metal ion study. J Arthroplasty 2011; 26: 511–518.
Li AE, Sneag DB, Miller TT, Lipman JD, Padgett DE, Potter HG. MRI of polyethylene tibial inserts in total knee arthroplasty: Normal and abnormal appearances. Am J Roentgenol. 2016; 206(6): 1264-1271.
Mistry A, Cahir J, Donell ST, Nolan J, Toms AP. MRI of asymptomatic patients with metal-on-metal and polyethylene-on-metal total hip arthroplasties. Clinical Radiology 2011; 66: 540-545.
Nawabi DH, Hayter CL, Su EP, Koff MF, Perino G, Gold SL, Koch KM, Potter HG. Magnetic resonance imaging findings in symptomatic versus asymptomatic subjects following metal-on-metal hip resurfacing arthroplasty. J Bone Joint Surg Am 2013; 95(10): 895-902.
Nawabi DH, Gold S, Lyman S, Fields K, Padgett DE, Potter HG. MRI predicts ALVAL and tissue damage in metal-on-metal hip arthroplasty. Clin Orthop Relat Res 2014; 472(2): 471–481.
Nawabi DH, Do HT, Ruel A, Lurie B, Elpers ME, Wright T, Potter HG, Westrich GH. Comprehensive analysis of a recalled modular total hip system and recommendations for management. J Bone Joint Surg Am 2016; 98(1): 40-47.
Nikolaou VS, Petit A, Khoury V, Blain-Pare E, Zukor DJ, Huk OL, Antoniou J. Magnetic resonance imaging of painful metal-on-metal total hip replacement. Eur J Orthop Surg Traumatol. 2015; 25(2): 313-9.
Nodzo SR, Esposito CI, Potter HG et al. MRI, retrieval analysis, and histologic evaluation of adverse total tissue reaction in metal-on-polyethylene total hip arthroplasty. J Arthroplasty (in press)
Nwawka OK, Konin GP, Sneag DB, Gulotta LV, Potter HG. Magnetic resonance imaging of shoulder arthroplasty: A review article. HSS J. 2014; 10 (3): 213 – 224.
Pandit H, Glyn-Jones S, McLardy-Smith P, Gundle R, Whitwell D, Gibbons CL, Ostlere S, Athanasou N, Gill HS, Murray DW. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br 2008; 90: 847–851.
Shulman RM, Zywiel MG, Gandhi R, Davey JR, Salonen DC. Trunnionosis: the latest culprit in adverse reactions to metal debris following hip arthroplasty. Skeletal Radiology 2015; 44: 433–440.
Silverman EJ, Ashley B, Sheth NP. Metal-on-metal total hip arthroplasty: Is there still a role in 2016? Curr Rev Musculoskelet Med 2016; 9: 93–96.
Thomas MS, Wimhurst JA, Nolan JF, Toms AP. Imaging Metal-on-Metal Hip Replacements: the Norwich Experience. HSS J 2013; 9(3): 247-56.
Toms AP, Marshall TJ, Cahir J, Darrah C, Nolan J, Donell ST, Barker T, Tucker JK. MRI of early symptomatic metal-on-metal total hip arthroplasty: a retrospective review of radiological findings in 20 hips. Clin Radiol 2008; 63: 49–58.
Yanny S, Cahir JG, Barker T, Wimhurst J, Nolan JF, Goodwin RW, Marshall T, Toms AP. MRI of aseptic lymphocytic vasculitis-associated lesions in metal-on-metal hip replacements. Am J Roentgenol. 2012; 198(6): 1394-402.
Figures