PI-RADS: NO!
1Department of Radiology, Ghent University Hospital, Ghent, Belgium
Synopsis
Reporting prostate MRI may be complex and prone to subjective interpretation. In 2012 the Prostate Imaging Reporting and Data System (PI-RADS) was introduced. The aims of PI-RADS were to provide minimal requirements for high-quality image acquisition, to standardize reporting, to simplify interpretation, to reduce inter-observer variability and to improve the accuracy of detecting clinically significant prostate cancer. In this lecture it is demonstrated that PI-RADS does not (yet) achieve these goals successfully and that other prostate MRI scoring systems show similar diagnostic performance. PI-RADS has its merits but requires further refinements.
Introduction: Reporting prostate MRI may be complex and prone to subjective interpretation. In 2012 the ESUR (European Society of Urogenital Radiology) guidelines on multiparametric prostate MRI (mpMRI) were published and the Prostate Imaging Reporting and Data System (PI-RADS) was introduced. In 2016 this system was adopted by the ACR (American College of Radiology) and an updated version of PI-RADS (PI-RADSv2) was developed. The objectives of PI-RADS were to provide minimal requirements for high-quality image acquisition, to standardize reporting, to simplify interpretation, to reduce inter-observer variability and to improve the accuracy of detecting clinically significant prostate cancer. In this lecture it is demonstrated that PI-RADS did not (yet) achieve these goals successfully.
Provide minimal requirements for high-quality image acquisition: In the PI-RADS guidelines Dynamic Contrast Enhanced Imaging (DCE) is recommended in all patients although its added value over T2-Weighted Imaging (T2-WI) and Diffusion Weighted Imaging (DWI) seems currently to be limited.
Standardization of reporting: PI-RADSv2 provides explicit criteria to score each sequence and provides consistent instructions to determine the overall assessment category on a scale from 1 to 5. An overall assessment score of 3 indicates that the findings are indeterminate but clarification of the cutoff value is needed for different clinical scenarios because in the end the clinician needs a binary recommendation for further diagnostic procedures (i.e. to biopsy or not).
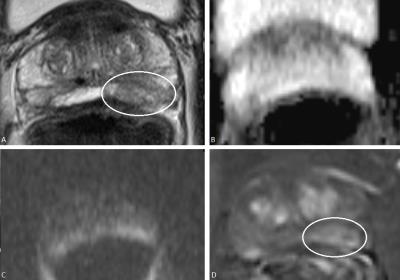
Simplify interpretation: Characterization of lesions with mpMRI remains difficult because the different pulse sequences may yield discordant results. The dominant sequence approach which is proposed in PI-RADSv2 may be an oversimplification because all sequences should be taken into account when interrogating a lesion. A possible method of improvement could be to define optimal weighting factors for each sequence.
Reduce inter-observer variability: The inter-observer variability of PI-RADS has been evaluated in several studies but appears to be rather moderate.
Improve the diagnostic accuracy of prostate MRI: PI-RADS aims to detect or exclude clinically significant prostate cancers but prostate MRI has its inherent limitations because small tumors may be missed (even if they are high grade) and benign mimickers may cause false positive results. Moreover the PI-RADS score is purely MRI derived although clinical factors such as age and comorbidity should be taken into account to determine the clinical significance of a prostate cancer.
Alternative scoring systems: many other scoring systems for prostate MRI have been described in the literature, such as the Likert scale (a subjective 5-point scoring system dependent on the radiologist’s overall impression), MLS (a 13-level score based on Morphology, Location and Signal intensity of a lesion), or local institutional scoring systems of e.g. Pinto (in which each parameter is categorized positive or negative in binary fashion), Rastinehad (SQS score) and De Visschere (PI-RADSv2Alt, based on DWI instead of DCE for upgrading T2-WI in the PZ). Reports of direct comparisons of these alternative scoring systems show similar diagnostic performance as PI-RADS.
Conclusion: PI-RADSv2 has its merits but does not (yet) achieve its goals and further refinements are required.
Acknowledgements
No acknowledgement found.References
1. Weinreb JC, Barentsz JO, Choyke PL, Cornud F, Haider MA, Macura KJ, et al. PI-RADS Prostate Imaging - Reporting and Data System: 2015, Version 2. European urology. 2016;69(1):16-40. doi: 10.1016/j.eururo.2015.08.052.
2. Westphalen AC, Rosenkrantz AB. Prostate imaging reporting and data system (PI-RADS): reflections on early experience with a standardized interpretation scheme for multiparametric prostate MRI. AJR American journal of roentgenology. 2014;202(1):121-3. doi: 10.2214/AJR.13.10889.
3. Rosenkrantz AB, Lim RP, Haghighi M, Somberg MB, Babb JS, Taneja SS. Comparison of interreader reproducibility of the prostate imaging reporting and data system and likert scales for evaluation of multiparametric prostate MRI. AJR American journal of roentgenology. 2013;201(4):W612-8. doi: 10.2214/AJR.12.10173.
4. Vargas HA, Hotker AM, Goldman DA, Moskowitz CS, Gondo T, Matsumoto K, et al. Updated prostate imaging reporting and data system (PIRADS v2) recommendations for the detection of clinically significant prostate cancer using multiparametric MRI: critical evaluation using whole-mount pathology as standard of reference. European radiology. 2015. doi: 10.1007/s00330-015-4015-6.
5. Muller BG, Shih JH, Sankineni S, Marko J, Rais-Bahrami S, George AK, et al. Prostate Cancer: Interobserver Agreement and Accuracy with the Revised Prostate Imaging Reporting and Data System at Multiparametric MR Imaging. Radiology. 2015;277(3):741-50. doi: 10.1148/radiol.2015142818.
6. Rosenkrantz AB, Babb JS, Taneja SS, Ream JM. Proposed Adjustments to PI-RADS Version 2 Decision Rules: Impact on Prostate Cancer Detection. Radiology. 2016:161124. doi: 10.1148/radiol.2016161124.
7. Rouviere O, Papillard M, Girouin N, Boutier R, Rabilloud M, Riche B, et al. Is it possible to model the risk of malignancy of focal abnormalities found at prostate multiparametric MRI? European radiology. 2012;22(5):1149-57. doi: 10.1007/s00330-011-2343-8.
8. Woo S, Suh CH, Kim SY, Cho JY, Kim SH. Diagnostic Performance of Prostate Imaging Reporting and Data System Version 2 for Detection of Prostate Cancer: A Systematic Review and Diagnostic Meta-analysis. European urology. 2017. doi: 10.1016/j.eururo.2017.01.042.
9. Pinto PA, Chung PH, Rastinehad AR, Baccala AA, Jr., Kruecker J, Benjamin CJ, et al. Magnetic resonance imaging/ultrasound fusion guided prostate biopsy improves cancer detection following transrectal ultrasound biopsy and correlates with multiparametric magnetic resonance imaging. The Journal of urology. 2011;186(4):1281-5. doi: 10.1016/j.juro.2011.05.078.
10. Portalez D, Mozer P, Cornud F, Renard-Penna R, Misrai V, Thoulouzan M, et al. Validation of the European Society of Urogenital Radiology scoring system for prostate cancer diagnosis on multiparametric magnetic resonance imaging in a cohort of repeat biopsy patients. European urology. 2012;62(6):986-96. doi: 10.1016/j.eururo.2012.06.044.
11. De Visschere PJ, Naesens L, Libbrecht L, Van Praet C, Lumen N, Fonteyne V, et al. What kind of prostate cancers do we miss on multiparametric magnetic resonance imaging? European radiology. 2016;26(4):1098-107. doi: 10.1007/s00330-015-3894-x.
12. De Visschere P, Lumen N, Ost P, Decaestecker K, Pattyn E, Villeirs G. Dynamic contrast-enhanced imaging has limited added value over T2-weighted imaging and diffusion-weighted imaging when using PI-RADSv2 for diagnosis of clinically significant prostate cancer in patients with elevated PSA. Clinical radiology. 2017;72(1):23-32. doi: 10.1016/j.crad.2016.09.011.
13. Rastinehad AR, Waingankar N, Turkbey B, Yaskiv O, Sonstegard AM, Fakhoury M, et al. Comparison of Multiparametric MRI Scoring Systems and the Impact on Cancer Detection in Patients Undergoing MR US Fusion Guided Prostate Biopsies. PLoS One. 2015;10(11):e0143404. doi: 10.1371/journal.pone.0143404.
14. Puech P, Rouviere O, Renard-Penna R, Villers A, Devos P, Colombel M, et al. Prostate cancer diagnosis: multiparametric MR-targeted biopsy with cognitive and transrectal US-MR fusion guidance versus systematic biopsy--prospective multicenter study. Radiology. 2013;268(2):461-9. doi: 10.1148/radiol.13121501.
15. Vache T, Bratan F, Mege-Lechevallier F, Roche S, Rabilloud M, Rouviere O. Characterization of prostate lesions as benign or malignant at multiparametric MR imaging: comparison of three scoring systems in patients treated with radical prostatectomy. Radiology. 2014;272(2):446-55. doi: 10.1148/radiol.14131584.
16. Rosenkrantz AB, Ginocchio LA, Cornfeld D, Froemming AT, Gupta RT, Turkbey B, et al. Interobserver Reproducibility of the PI-RADS Version 2 Lexicon: A Multicenter Study of Six Experienced Prostate Radiologists. Radiology. 2016:152542. doi: 10.1148/radiol.2016152542.
17. Hamoen EH, de Rooij M, Witjes JA, Barentsz JO, Rovers MM. Use of the Prostate Imaging Reporting and Data System (PI-RADS) for Prostate Cancer Detection with Multiparametric Magnetic Resonance Imaging: A Diagnostic Meta-analysis. European urology. 2015;67(6):1112-21. doi: 10.1016/j.eururo.2014.10.033.
18. Rosenkrantz AB, Kim S, Lim RP, Hindman N, Deng FM, Babb JS, et al. Prostate cancer localization using multiparametric MR imaging: comparison of Prostate Imaging Reporting and Data System (PI-RADS) and Likert scales. Radiology. 2013;269(2):482-92. doi: 10.1148/radiol.13122233.
19. Schimmoller L, Quentin M, Arsov C, Lanzman RS, Hiester A, Rabenalt R, et al. Inter-reader agreement of the ESUR score for prostate MRI using in-bore MRI-guided biopsies as the reference standard. European radiology. 2013;23(11):3185-90. doi: 10.1007/s00330-013-2922-y.
20. de Rooij M, Hamoen EH, Futterer JJ, Barentsz JO, Rovers MM. Accuracy of multiparametric MRI for prostate cancer detection: a meta-analysis. AJR American journal of roentgenology. 2014;202(2):343-51. doi: 10.2214/AJR.13.11046.
21. Barentsz JO, Weinreb JC, Verma S, Thoeny HC, Tempany CM, Shtern F, et al. Synopsis of the PI-RADS v2 Guidelines for Multiparametric Prostate Magnetic Resonance Imaging and Recommendations for Use. European urology. 2016;69(1):41-9. doi: 10.1016/j.eururo.2015.08.038. 22. Barentsz JO, Richenberg J, Clements R, Choyke P, Verma S, Villeirs G, et al. ESUR prostate MR guidelines 2012. European radiology. 2012;22(4):746-57. doi: 10.1007/s00330-011-2377-y.
23. Rosenkrantz AB, Margolis DJ. Commentary regarding the inter-reader reproducibility of PI-RADS version 2. Abdom Radiol 2016;41:907-909. Doi: 10.1007/s00261-0756-1
24. Rosenkrantz AB, Oto A, Turkbey B, Westphalen AC. Prostate Imaging Reporting and Data System (PI-RADS), Version 2: A Critical Look. AJR 2016;206:1179-1183. Doi: 10.2214/AJR.15.15765
Figures