Gadolinium Safety & Deposition: Past, Present, & Future
1Radiology, Ohio State University, Columbus, OH, United States
Synopsis
The jarring clinical facts of NSF and the recent detection by MRI (an insensitive tool) of gadolinium in the dentate nucleus of the brain have brought GBCA stability and Gd deposition to attention. Numerous recent studies are contributing to a more thorough understanding of in vivo chemical deposition and pharmacokinetics and speciation of GBCA, and will soon stimulate studies to more deeply understand the toxicology of those species. This lecture will describe basic design and function principles and historical development of the GBCA emphasizing the links between chemical structure and gadolinium dissociation and deposition.
Basic Structure and Function of GBCA
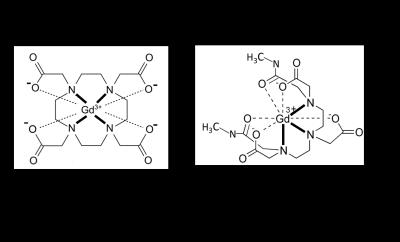
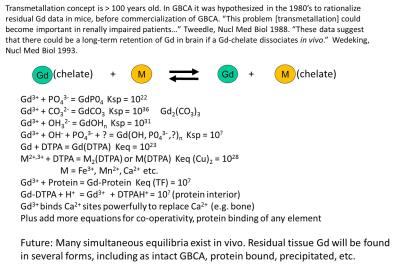
A few chemical concepts are needed to support the discussion of the Gd based contrast agents (GBCA). There must be very strong chemical bonds between the chelating agent and the metal ion (Figure 1). (1) Let us recall that thermodynamic stability constants describe the energy (and entropy) that is involved in making and breaking of all of the bonds in a Gd chelate. The larger the magnitude of Keq or Kf’ (Keq adjusted to physiologic pH), the more tendency that the equilibrium, Gd3+ + chelate = Gd(chelate), is driven to the right. GBCA are all extraordinarily driven rightward toward chelation, by typically 15 – 20 orders of magnitude. That is the purpose of the chelate, and for good reason since the free ion of Gd is insoluble at physiologic pH and toxic at high concentrations. The situation in vivo is anything but simple, as there are numerous competitors of Gd for the chelating ligand (e.g. endogenous metals), competitors of the chelating ligand for the Gd3+ ion (e.g. phosphate, hydroxide), and metabolizing enzymes (Figure 2). All of these equilibria operate simultaneously, and given enough time, any Gd(chelate) will lose the battle. But while this harsh milieu creates pressure on the GBCA, there are two additional protections: 1) the rapid rate at which the GBCA is being excreted into the urine (90 min halftime), and 2) the fact that all those connected bonds to Gd work together, making dissociation of Gd a slow process. What makes the two structural archetypes in Figure 1 different is not their Keq or Kf’ values. Their overall fate on the battlefield in vivo is the same. What is different is the rate at which they will lose to the simultaneous multiple competitors. The rate of the dechelation is governed intrinsically by the slowest micro process, which is the breaking of the Gd-N bonds. In the macrocycles that process requires a very nearly simultaneous breaking of all four Gd-N bonds, an extraordinarily unlikely event, due to the rigid ring connecting them. In the linear structure it is possible for the competitors to peel one N at a time away from the Gd ion without as much resistance of the rest of the backbone structure. Thermodynamics is not useless, but it is only predictive of the final equilibrium, which commercial GBCA never reach. Keq and Kf’ cannot predict the in vivo dissociation of Gd(chelates) even among linear backboned molecules, overall. Gd(EDTA) has almost the same Kf’ as gadodiamide, Gd(DO3A), gadobutrol and others, and yet Gd(EDTA) is highly toxic, losing half of its Gd immediately on injection, while the others are acutely stable with high LD50 values in mice.Hierarchy of of the Relevance of Data
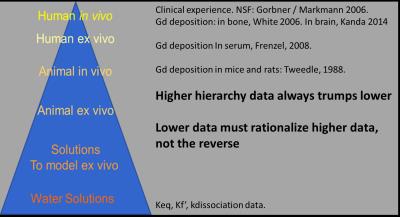
As we discuss GBCA development and Gd deposition historically, it is important to recognize that the data exist within a hierarchy that must be respected as we discuss the topic and draw conclusions (Figure 3). At the highest point are data obtained in vivo from human subjects: e.g. the elevated MRI signal intensity observed in the dentate nucleus (2) and the existence of NSF (nephrogenic systemic fibrosis) in association with the administration of commercial GBCA. (3) While nuances exist, human in vivo data are more relevant to clinical use of GBCA than data obtained ex vivo from human tissues, which in turn are more relevant than animal data. At the bottom of the hierarchy are data on the chemistry, like stability constants or kinetics of dissociation of Gd(chelate) obtained in non-biological media, and computer simulations using these data. (4-6) The primary purpose of obtaining data lower on the hierarchy is to rationalize more important data higher up the hierarchy. When discrepancy exists between two valid sets of data, it behooves us to question the relevance of the rationalization of the connection. An example that the NSF era finally destroyed was the rationalization that Gd(chelates) with greater thermodynamic stability constants are more “stable” and therefore safer.Brief History of GBCA
Condensing the rich 40 year history of MRI contrast agents into a very small space, I apologize for inevitable loss of granularity and slights to major contributors. In 1978 the Lauterbur group published on the first MRI contrast agent, the Mn2+ ion that could enhance a canine heart by virtue of its natural uptake mechanism. (7) The work interested Schering AG enough that they began a project to create a safe, injectable paramagnetic agent, ending up deciding in favor of Gd(DTPA) that eventually became commercial gadopentetate a decade later. They filed a patent, of course, in 1981 that was considered pioneering by the USPTO and given broad claims that were licensed by all other companies who made gadodiamide, gadoteridol, gadoterate, etc. They also hedged their bet by funding academic research into alternatives, like nitroxides. However, the nitroxides, which bore no metals were all far less effective on a mole dose basis at enhancing MRI scans, having a single unpaired electron versus 7 for Gd3+. Also less effective were alternative metals, Mn2+, Fe3+, with 5 unpaired electrons. Pharmaceutical parameters usually involved in tolerance testing contrast agents for X ray imaging, which were delivered at tenfold higher doses, were tested and the ratio of tolerance per dose was the same for Gd(chelates) as it was for iopamidol and iohexol, the nonionic X ray agents. Gd(III) had the additional advantage that it was available only in a single oxidation state, unlike Mn(II) and Fe(III), and as such could not engage in redox chemistry, like the Fenton chemistry that produces radicals with Fe(II). All three bare metals were toxic at the mole doses required for MRI. Even when, later on, mangafodapir was used to image the free Mn2+ ion, it had to be chelated for initial injection. Free Gd did not become an issue except in a few chemists’ minds in the late 1980’s. They demonstrated between 1988 and 1995 that some small amounts of Gd (0.03 – 0.3 % of the injected MRI level dose) remained residual 1 -2 weeks after dosing in mice, and that endogenous ions could aid dissociation of Gd in vitro, with the macrocycle being more resistant. (8-11) These studies detected long lived Gd, but did not detect dissociated Gd directly. Residual Gd was more demonstrably dissociated from a linear GBCA in rats by a dual radiolabeling technique. (12) Radiolabeled GBCA did not demonstrate brain 153Gd above LOD, but interesting in the context of today’s plenary topic, injected free 153Gd (as the acetate) showed brain deposition with very slow to no clearance, while in the whole mice free Gd3+ cleared at a T1/2 of ~ 50 days. (13) Human skull bone chips were found to be 0.1 – 0.8 ppm in Gd in 1990 after gadopentetate injections but the LOD was “1 ppm” and judged “insignificant.” (14) That some Gd was released from gadopentetate in humans from that agent’s earliest formulation was deducible, related to transient, reversible Fe and bilirubin elevations in human blood samples, because adding additional chelating agent to the formulation was the remedy. (15) The formulation of gadodiamide (which showed the same transient elevations in clinical trials) were fortified with 5 mol % of additional chelating agent from the beginning, and this increased the LD50 in mice (6) and reduced the residual Gd remaining in mice after dosing. (9) Prior to NSF connection to Gd in 2006, macrocyclic agents were shown in vitro, in animals and then finally in human bone fragments (16) to lead to lower residual Gd. (But in 2009 Darrah (17) found for the same two agents, no macrocycle vs linear GBCA difference in bone 8 years after exposure). While the weight of the evidence favors dissociated Gd as highly probable, it was not directly detected by 2006. In 2006, it was discovered that a very rare disease, NSF, was connected to the use of linear GBCA in patients with severe renal impairment. (3) Since then it is now known that the order of decrease from most cases to least cases follows the order of the known residual Gd from the studies above, strongly inferring, though still not proving, that it is dissociated Gd that is the trigger. Notably, only 5% of patients with severe renal impairment and the high risk GBCA actually acquired known NSF, suggesting that a third, unknown element must be present. Dissociated Gd was implied as causative when Frenzel measured GBCA stability in serum, finding that all three macrocycles had no detectable dissociated Gd, while dissociation was clearly demonstrated in all linear GBCA.(18) The fact that contraindicating linear GBCA, except for gadobenate that uniquely has an added hepatobiliary path to excretion with otherwise mostly renal excretion, stopped NSF, contributes to the free Gd hypothesis. Dissociated Gd was also found in skin tissue of an NSF patient, where Birka found insoluble Gd, plus gadoteridol, but not gadopentetate, years after dosing the two agents. (19) Gd in biopsy samples was found paired with Ca and P, suggesting GdPO4 deposition. With the peak hierarchy fact of NSF added to the medical and toxicologic knowledge base, there was finally serious clinical attention paid to the Gd dissociation phenomenon. Probably this awareness played a role in Kanda’s discovering, in 2014, elevated MRI signal in an area of the brain known to concentrate metal ions, the dentate nucleus. Subsequent studies on ex vivo human autopsy tissue have demonstrated that Gd was indeed present in the brain tissue, the MRI signal correlated to dose, the highest and lowest (or no) signal ordering of GBCA showed that macrocycles have the smallest effect, and also no H&E pathology was obvious. (20-22)Selected Recent Studies
With this historical perspective we can see that there was early evidence to suggest “Gd brain deposition” except not for exactly where (dentate nucleus, etc.), not in humans, and not how (by MRI) Gd is being detected. What makes the recent findings especially significant is that MRI is a rather insensitive tool to detect Gd, and that neural tissue is toxicologically sensitive. Whether the Gd in the DN is intact GBCA or dissociated Gd, or both, it is located in a very deep pharmacokinetic compartment from the point of view of eventual excretion (i.e. much slower), so that patients needing multiple doses of GBCA are able to build up to the ~10 uM [Gd] required to detect Gd (compared to neighboring tissue) by MRI. (23) The phenomenon is complicated by the fact that other paramagnetic metals are no doubt present, and that the studies are retrospective, and have therefore obvious inherent weaknesses. A look into the raw data in the studies points to a wide variation in effect, probably in part related to the variations in the times between the multiple doses while at least any chelated intact GBCA is slowing clearing the brain, and if the mice experiments are predictive, even the dissociated Gd is clearing the body, but perhaps also entering the CNS as it did in the mice. The brain deposition is now attracting a great deal of attention, (24) (systematic review) and causing changes of specific GBCA use, as did NSF, in the hopes that a similar toxicologic outbreak of GBCA side effects as from NSF can be avoided. But is there any evidence to suggest that longer exposure to GBCA and even dissociated Gd at the low levels detected will manifest itself in important toxicity? One thing not clarified in the retrospective human MRI and the human autopsy studies is what fraction of any retained Gd is simply slowly clearing intact GBCA, and probably (?) harmless. It is possible that in Birka’s NSF patient, the GBCA was truly trapped in the poorly perfused skin. Two well executed recent rat studies are relevant. One showed that ~50 % of very heavily dosed (12 mmol/kg) gadodiamide cleared the brain over 20 weeks with no H&E neurotoxicity. (25) In a similar but not identical study even more heavily dosed (25 mmol/kg) rat study, ~50% of the same GBCA was found in insoluble and protein bound brain fractions. (26) Protein bound Gd can have a vastly stronger effect on MRI signal that GBCA or insoluble Gd. (1) In the latter study, it was found that three linear agents showed the same speciation, but that only soluble small molecules were detected for the two macrocycles. The mechanisms for brain uptake and clearance are several and complex, and both directions of movement and their kinetics will need to be considered. Another relevant subject will be the findings of Gd in non neural tissue, for example, in up to 23 fold greater amounts in bone compared to brain. (27)Toxicologic History and Questions
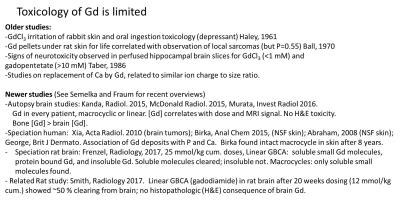
The toxicology history for Gd is not very rich, probably because there is not much to find, but it is partially documented in Figure 4, and in recent reviews.(28, 29) Very long term exposure to implanted Gd (metal in oxidation state, 0, not 3+ ion) might have been associated with rat sarcoma formation (but without significance). (30) It was demonstrated GdCl3 was irritating to rabbit skin. (31) More relevant to GBCA per se, it took 10 mM gadopentetate to observe neurotoxicity in perfused hippocampal brain slices, but < 1 mM GdCl3. (32) To analyze the link between toxicity and free Gd in Gd deposition in brain, we must first find some toxicity there, which will probably be easier to do with dissociated Gd than intact GBCA. Speciation and toxicology of GBCA and free Gd species are needed. Luckily, the tools exist, laser ablation ICP-MS, hydrophilic extraction HPLC, and MALDI imaging, even if inherent weaknesses exist, usually related to sample preparation. (33) It is well appreciated by toxicologists that histopathology with H&E is a first step, but fairly insensitive. What possibilities exist for subtle chronic toxicologic effects? Should all toxicology of new drugs be published? What amount of Gd / GBCA/ AUC is insignificant? Are Fe(III) and/or Mn(II) safer agents? These are complex and expensive questions. We should bear in mind as we search for toxicity of Gd, what concentration is the relevant range with whatever GBCA are being used, and that GBCA have been extremely useful, and overall extremely safe over the past 30 years, after hundreds of million uses.Acknowledgements
The author acknowledges the Stefanie Spielman Foundation and the Wright Center for Innovation in Biomedical Imaging.References
1. Caravan P, Ellison JJ, McMurry TJ, Lauffer RB. Gadolinium(III) chelates as MRI contrast agents: Structure, dynamics, and applications. Chem Rev. 1999;99(9):2293-352. PubMed PMID: ISI:000082569800006.
2. Kanda T, Ishii K, Kawaguchi H, Kitajima K, Takenaka D. High signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted MR images: relationship with increasing cumulative dose of a gadolinium-based contrast material. Radiology. 2014;270(3):834-41. Epub 2014/01/31. doi: 10.1148/radiol.13131669. PubMed PMID: 24475844.
3. Grobner T. Gadolinium–a specific trigger for the development of nephrogenic fibrosing dermopathy and nephrogenic systemic fibrosis? Nephrol Dial Transpl. 2006;21(4):1104-8.
4. Jakovljevic I, Petrovic D, Joksovic L, Lazarevic I, Durdevic P. Computer Simulation of Speciation of Trivalent Aluminum, Gadolinium and Yttrium Ions in Human Blood Plasma. Acta Chimica Slovenica. 2013;60(4):861-9. PubMed PMID: WOS:000329194200018.
5. Hao D, Ai T, Goerner F, Hu X, Runge VM, Tweedle M. MRI contrast agents: Basic chemistry and safety. Journal of Magnetic Resonance Imaging. 2012;36(5):1060-71. doi: 10.1002/jmri.23725.
6. Cacheris WP, Quay SC, Rocklage SM. The relationship between thermodynamics and the toxicity of gadolinium complexes. Magnetic resonance imaging. 1990;8(4):467-81. Epub 1990/01/01. PubMed PMID: 2118207.
7. Lauterbur P, Mendonca Diaz, Rudin AM. Frontiers in Biomedical 1978.
8. Tweedle MF, Gaughan GT, Hagan J, Wedeking PW, Sibley P, Wilson LJ, Lee DW. Considerations Involving Paramagnetic Coordination-Compounds as Useful Nmr Contrast Agents. Nuclear Medicine and Biology. 1988;15(1):31-6. PubMed PMID: ISI:A1988L614900007.
9. Tweedle MF, Wedeking P, Kumar K. Biodistribution of radiolabeled, formulated gadopentetate, gadoteridol, gadoterate, and gadodiamide in mice and rats. Investigative radiology. 1995;30(6):372-80. Epub 1995/06/01. PubMed PMID: 7490190.
10. Tweedle M, Hagan J, Kumar K, Mantha S, Chang C. Reaction of gadolinium chelates with endogenously available ions. Magnetic resonance imaging. 1991;9(3):409-15.
11. Wedeking P, Kumar K, Tweedle MF. Dissociation of Gadolinium Chelates in Mice - Relationship to Chemical Characteristics. Magnetic resonance imaging. 1992;10(4):641-8. PubMed PMID: ISI:A1992JF73400016.
12. Kasokat T, Urich K. Quantification of Dechelation of Gadopentetate Dimeglumine in Rats. Arzneimittel-Forsch. 1992;42-1(6):869-76. PubMed PMID: ISI:A1992HZ89100022.
13. Wedeking P, Kumar K, Tweedle MF. Dose-Dependent Biodistribution of [Gd-153]Gd(Acetate)N in Mice. Nuclear Medicine and Biology. 1993;20(5):679-91. doi: Doi 10.1016/0969-8051(93)90039-W. PubMed PMID: ISI:A1993LK30300016. 14. Weinmann H-J, Press WR, Raduchel J, Platzek H, Schmitt-Willich H, Vogler H. Characteristics of Gd-DTPA and new derivatives. In: Bydder G, Felix r, Buchler E, Drayer BP, Niendorf HP, Takahashi M, Wolf K-J, Dinger JC, editors. Contrast Media in MRI The Netherlands: Medicom Europe, B.V.; 1990. p. 19-29.
15. Niendorf HP, Dinger JC, Haustein J, Cornelius I, Alhassan A, Clauss W. Tolerance of Gd-DTPA: clinical experience. In: Bydder GM, Felix R, Bucheler E, Drayer BP, Niendorf HP, Takahashi M, Wolf KJ, editors. Contrast Media in MRI. The Netherlands: Medicom Europe; 1990. p. 31-40.
16. White GW, Gibby WA, Tweedle MF. Comparison of Gd(DTPA-BMA) (Omniscan) versus Gd(HP-DO3A) (ProHance) relative-to gadolinium retention in human bone tissue by inductively coupled plasma mass spectroscopy. Investigative radiology. 2006;41(3):272-8. doi: DOI 10.1097/01.rli.0000186569.32408.95. PubMed PMID: ISI:000235632800010.
17. Darrah TH, Prutsman-Pfeiffer JJ, Poreda RJ, Ellen Campbell M, Hauschka PV, Hannigan RE. Incorporation of excess gadolinium into human bone from medical contrast agents. Metallomics : integrated biometal science. 2009;1(6):479-88. doi: 10.1039/b905145g. PubMed PMID: 21305156.
18. Frenzel T, Lengsfeld P, Schirmer H, Hutter J, Weinmann HJ. Stability of Gadolinium-Based Magnetic Resonance Imaging Contrast Agents in Human Serum at 37 degrees C. Investigative radiology. 2008;43(12):817-28. PubMed PMID: ISI:000261271300001.
19. Birka M, Wentker KS, Lusmoller E, Arheilger B, Wehe CA, Sperling M, Stadler R, Karst U. Diagnosis of Nephrogenic Systemic Fibrosis by means of Elemental Bioimaging and Speciation Analysis. Analytical chemistry. 2015;87(6):3321-8. Epub 2015/02/25. doi: 10.1021/ac504488k. PubMed PMID: 25708271.
20. Kanda T, Fukusato T, Matsuda M, Toyoda K, Oba H, Kotoku J, Haruyama T, Kitajima K, Furui S. Gadolinium-based Contrast Agent Accumulates in the Brain Even in Subjects without Severe Renal Dysfunction: Evaluation of Autopsy Brain Specimens with Inductively Coupled Plasma Mass Spectroscopy. Radiology. 2015;276(1):228-32. doi: 10.1148/radiol.2015142690. PubMed PMID: 25942417.
21. McDonald RJ, McDonald JS, Kallmes DF, Jentoft ME, Murray DL, Thielen KR, Williamson EE, Eckel LJ. Intracranial Gadolinium Deposition after Contrast-enhanced MR Imaging. Radiology. 2015:150025. Epub 2015/03/06. doi: 10.1148/radiol.15150025. PubMed PMID: 25742194.
22. Murata N, Gonzalez-Cuyar LF, Murata K, Fligner C, Dills R, Hippe D, Maravilla KR. Macrocyclic and Other Non-Group 1 Gadolinium Contrast Agents Deposit Low Levels of Gadolinium in Brain and Bone Tissue: Preliminary Results From 9 Patients With Normal Renal Function. Investigative radiology. 2016;51(7):447-53. doi: 10.1097/RLI.0000000000000252. PubMed PMID: 26863577.
23. Wedeking P, Shukla R, Kouch Y, Nunn A, Tweedle M. Utilization of the nephrectomized mouse for determining threshold effects of MRI contrast agents. Magnetic resonance imaging. 1999;17(4):569-75. 24. Olchowy C, Cebulski K, Lasecki M, Chaber R, Olchowy A, Kalwak K, Zaleska-Dorobisz U. The presence of the gadolinium-based contrast agent depositions in the brain and symptoms of gadolinium neurotoxicity - A systematic review. PloS one. 2017;12(2):e0171704. doi: 10.1371/journal.pone.0171704. PubMed PMID: 28187173; PMCID: PMC5302442.
25. Smith APL, Marino M, Roberts J, Crowder JM, Castle J, Lowery L, Morton C, Hibberd MG, Evans PM. Clearance of Gadolinium from the Brain with No Pathologic Effect after Repeated Administration of Gadodiamide in Healthy Rats: An Analytical and Histologic Study. Radiology. 2017;282(3):743-51.
26. Frenzel T, Apte C, Jost G, Schockel L, Lohrke J, Pietsch H. Quantification and Assessment of the Chemical Form of Residual Gadolinium in the Brain After Repeated Administration of Gadolinium-Based Contrast Agents: Comparative Study in Rats. Investigative radiology. 2017. doi: 10.1097/RLI.0000000000000352. PubMed PMID: 28125438.
27. Murata N, Gonzalez-Cuyar LF, Murata K, Fligner C, Dills R, Hippe D, Maravilla KR. Macrocyclic and other non–group 1 gadolinium contrast agents deposit low levels of gadolinium in brain and bone tissue: preliminary results from 9 patients with normal renal function. Investigative radiology. 2016;51(7):447-53. 28. Fraum TJ, Ludwig DR, Bashir MR, Fowler KJ. Gadolinium-based contrast agents: A comprehensive risk assessment. J Magn Reson Imaging. 2017. doi: 10.1002/jmri.25625. PubMed PMID: 28083913.
29. Semelka RC, Ramalho M, Jay M. Summary of special issue on gadolinium bioeffects and toxicity with a look to the future. Magnetic resonance imaging. 2016;34(10):1399-401. doi: 10.1016/j.mri.2016.09.002. PubMed PMID: 27639920.
30. Haley TJ, Raymond K, Komesu N, Upham HC. Toxicological and pharmacological effects of Gadolinium and samarium chlorides. Brit J Pharmacol. 1961;17:526-32.
31. Ball RA, Vangelde.G, Green JW, Reece WO. Neoplast Ic Sequelae Following Subcutaneous Implantation of Mice with Rare Earth Metals. P Soc Exp Biol Med. 1970;135(2):426-&. PubMed PMID: ISI:A1970H862700049.
32. Taber KH, Bryan RN. The Neurotoxicity of Agents that could be used for contrast-enhanced magnetic resonance imaging. In: Runge VR, Claussen C, Felix R, James AE, editors. Contrast Agents in Magnetic Resonance Imaging. Amsterdam: Excerpta Medica; 1986. p. 70 - 3.
33. Tweedle MF. Gadolinium deposition: Is it chelated or dissociated gadolinium? How can we tell? Magnetic resonance imaging. 2016;34(10):1377-82. doi: 10.1016/j.mri.2016.09.003. PubMed PMID: WOS:000389287000008.
Figures