Synopsis
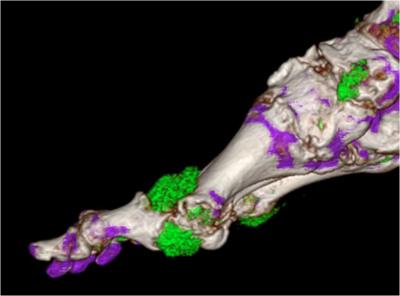
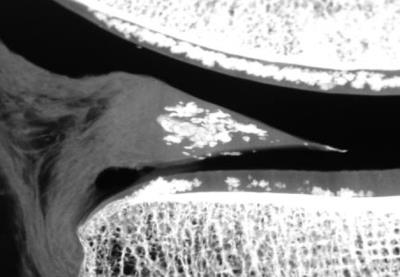
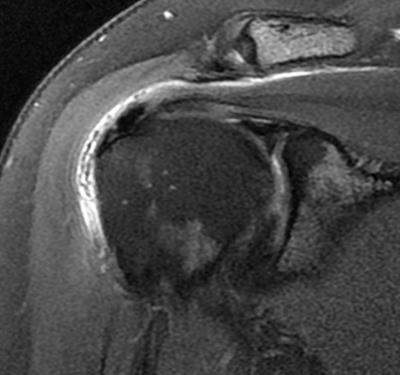
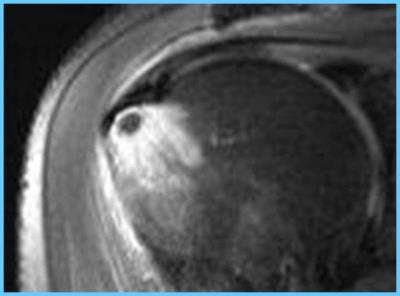
Several
crystals (urate, CPPD and hydroxyapatite) can deposit in tissues of the
musculoskeletal system in asymptomatic individuals. I in some cases, those
deposits can be associated with diseases such as Gout, Pseudogout and Calcific
Tendinitis. MRI examination can be very useful in the diagnosis of such
entities, differential diagnosis and help treatment decisions.
Acknowledgements
No acknowledgement found.References
Pascual E, Jovani V.
Synovial fluid analysis. Best Pract Res Clin Rheumatol.
2005;19:371-386.
2. Bond JR, Sim FH,
Sundaram M. Radiologic case study: Gouty tophus involving the distal quadriceps
tendon. Orthopedics. 2004;27:90-92.
3. Miller LJ, Pruett SW,
Losada R, et al. Tophaceous gout of the lumbar spine: MR findings. J
Computer Assisted Tomography. 1996;20:1004-1005.
4. Chen CKH, Yeh LR, Pan
HB, et al. Intra articular gouty tophi of the knee: CT and MRI imaging in 12
patients. Skeletal Radiology. 1999;28:75-80.
5. Yu JS, Chung C, Recht
M, et al. MR imaging of the tophaceous gout. AJR Am J Roengtgenol.
1997;168:523-527.
6. McCarty DJ, Hollander
JL. Identification of urate crystals in gouty synovial fluid. Ann
Intern Med. 1961; 54:452-460.
7. McCarty DJ, Kohn NN,
Faires JS. The significance of calcium pyrophosphate crystals in synovial fluid
of arthritis patients: the “pseudogout” syndrome. Ann Intern Med.
1962;56:711-737.
8. Zitnan D, Sitaj S.
Chondrocalcinosis polyarticularis (familiaris): Roentgenological and clinical
analysis.Cesk Rentgenol. 1960;14:27-34.
9. Timms AE, Zhang Y,
Russell RG, Brown MA. Genetic studies of disorders of calcium crystal deposition. Rheumatology.
2002;41:725-729.
10. Scotchford CA,
Greenwald S, Ali SY. Calcium phosphate crystal distribution in the superficial
zone of human femoral head articular cartilage. J Anat.
1992;181:293-300.
11. Doherty M, Dieppe P,
Watt I. Low incidence of calcium pyrophosphate dihydrate crystal deposition in
rheumatoid arthritis, with modification of radiographic featuers in coexistent
disease. Arthritis Rheum. 1984; 27:1002-1009.
12. Steinbach LS, Resnick
D. Calcium pyrophosphate dihydrate crystal deposition disease revisited. Radiology.
1996;200:1-9.
13. Giachelli CM. Inducers
and inhibitors of biomineralization: Lessons from pathological
calcification. Orthod Craniofacial Res. 2005;8:229-231.
14. Jim YF, Hsu HC, Chang
CY, et al. Coexistence of calcific tendonitis and rotator cuff tear: An arthrographic
study. Skeletal Radiol. 1993;22: 183-185.
15. Zubler, C, Mengiardi
B, Schmid MR, et al. MR arthrography in calcific tendinitis of the shoulder:
Diagnostic performance and pitfalls. Eur Radiol. 2007;17:1603-1610.
16. Wasserman E, Richman
A, Erdag N, Weiss R. Acute calcific prevertebral tendonitis of the longus colli
muscle. Applied Radiology. 2009;38:169.
17. Offiah, CE, Hall E.
Acute calcific tendinitis of the longus colli muscle: Spectrum of CT
appearances and anatomical correlation. Br J Radiol. 2009;82:117-121.
18. Farpour F, Phan SJ,
Burns J, Tehranzadeh J. Enhanced MR imaging of the shoulder, and
sternoclavicular and acromioclavicular joint arthritis in primary
hemochromatosis. Rheumatol Int. 2011;31:395-398. Epub 2009 Oct
14.