5548
Non-contrast-enhanced imaging of RF ablation lesions in the heart1Division of Cardiology, Johns Hopkins University, School of Medicine, Baltimore, MD, United States, 2Department of Biomedical Engineering, Johns Hopkins University, School of Medicine, Baltimore, MD, United States
Synopsis
Non-contrast-enhanced T1-weighted imaging has been demonstrated to be an effective technique for visualization of acute RF ablation lesions in the heart. Current practice does not include any soft tissue visualization, which could lead to gaps or incomplete ablations and possible recurrence of symptoms. We propose a T1-weighted sequence with long TI to increase contrast between normal and ablated myocardium. Images are presented demonstrating the technique after ablations in the ventricles, left atrium and pulmonary vein.
Introduction
T1-weighted (T1w) MR imaging has been demonstrated to provide positive contrast for visualizing radio-frequency ablation (RFA) lesions.1 This may be valuable in assessment of treatment, during or after a procedure. In current procedures, visualization of soft tissue is not available, increasing the possibility of leaving gaps or incomplete ablations in target regions. This may lead to cases of recurrence in some patients.
In this work, we show examples from ablations performed in ventricular or atrial myocardium, as well as pulmonary vein (PV), where electrical isolation is attempted in some atrial fibrillation patients. Examples are also shown from experiments where ablations were performed against a background of scar from myocardial infarction (MI). The results indicate that this non-contrast-enhanced imaging technique may be useful in many regions of the heart.
Methods
In six normal naive swine, both left and right ventricles were ablated. In three swine, ablation lesions were created in the left atrium (LA), and in the right superior pulmonary vein (RSPV) to emulate an attempt at electrical isolation of a PV. In three swine, MI was induced by 120 min balloon occlusion of the LAD. Eight weeks post-MI, delayed contrast enhanced (DCE) imaging was performed to produce a substrate map. RFA was targeted at infarct border zones using electro-anatomical mapping and the substrate map.
Imaging was performed after RFA using a free-breathing navigator-gated 3D inversion recovery sequence for T1-weighting. A long TI (~700 ms) was used to maximize contrast between lesions and normal myocardium, requiring 2-beat triggering for higher heart rates. Typical imaging parameters were: flip=25 deg, TR/TE=5.4/2.7 ms, pixel size=1.1x1.1x2.5 mm, BW=250 Hz/pixel, 32-40 slices, scan time=10-15 min. Additional higher resolution images (pixel size=1.1x1.1x2.2 mm interpolated to 1.1 mm isotropic) required ~20 minutes. DCE imaging with similar resolution was also performed.
Results
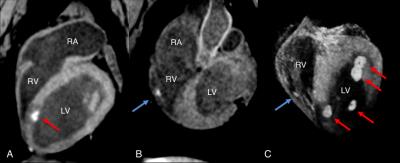
Swine with ventricular ablations: In all experiments, RFA lesions were clearly evident in the non-contrast T1w scans in both LV and thin RV walls (Fig. 1A,B). Lesion core is hyperenhanced and surrounded by a hypo-intense ring. TI between 700-900 ms produced best contrast between lesion and normal myocardium, with the lower range providing better blood suppression, improving lesion conspicuity. CNR was sufficient to create 3D volume renderings using cropping and window/level adjustment (Fig. 1C).
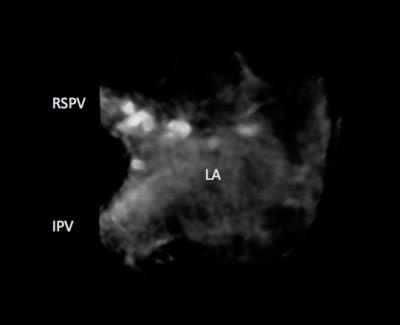
Swine with atrial ablations: In all experiments, enhancement of lesion cores in atrial myocardium and RSPV were evident in the non-contrast-enhanced images (Fig. 2). Better quality was seen in the higher resolution acquisition. The hypo-intense ring was not as evident.
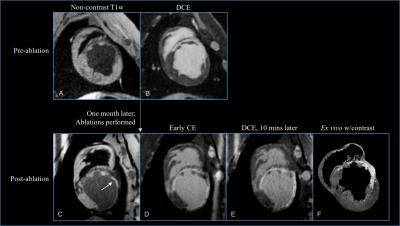
Swine with MI: Chronic scar tissue appeared hypo-enhanced in the T1w images (Fig. 3). Enhancement of acute lesion cores was readily visible against scar (C), and lesion extent was apparently limited by the scar. In early phase DCE (D), lesion core appeared hypo-enhanced while scar was enhanced. In later phase DCE (E, 10 mins later), acute lesion cores and chronic scar were both enhanced and not distinguishable from each other.
Discussion
This non-contrast-enhanced T1w imaging technique provides positive contrast for visualization of RFA lesions. In all experimental scenarios we tried, the same imaging parameters produced excellent contrast between normal myocardium and lesion core.
When substrate is scarred, specificity is improved with T1w over DCE since acute RFA lesions are enhanced and chronic scar is hypo-enhanced. Specificity is maintained with T1w, whereas contrast agent distribution is continuously changing in DCE scans.
Since the proposed T1w imaging technique does not require contrast agent, images can be re-acquired as needed. Whereas a contrast-enhanced protocol may be executed only once or twice in a session and provides a time-evolving enhancement pattern which can confound image interpretation.
Conclusion
Non-contrast-enhanced T1w imaging with long TI provides readily visible contrast for visualization of acute RFA lesions in ventricles, LA or PV.
Acute ablations adjacent to chronic scar are conspicuous with good specificity, since the acute lesion is enhanced, and the chronic scar is hypo-enhanced.
Acknowledgements
Grant support: NIH R01 HL094610, NIH R01 HL126092, NIH R21 EB023515References
1. Guttman M, Tao S, Kolandaivelu A, Halperin H, Herzka H. Non-contrast-enhanced imaging of radiofrequency ablation lesions in normal and infarcted myocardium. J Cardiovasc Magn Reson, In Press.
Figures