5543
The role of in-bore MR-guided prostate biopsies in patients With discrepancy between MRI findings and TRUS biopsies1Departement of Radiology and Nuclear Medicine, St Olavs Hospital, Trondheim, Norway, 2Department of Pathology and Genetics, St Olavs Hospital, Trondheim, Norway, 3Department of Circulation and Medical Imaging, Norwegian University of Science and Technology, Trondheim, 4Departement of Urology, St Olavs Hospital, Trondheim, Norway
Synopsis
A retrospecive review of 34 patients who had been to former TRUS guided prostate biopsies, where there was a discrepancy between MRI reported tumor suspicious findings and histology. They were re-biopsied with MRGB. We could verify cancer in 14 of 24 patients with former negative or benign histology. We also upgraded 7 out of 10 patients from low-grade to intermidiate or high-grade cancer. In addition to finding former unknown cancers, we also found that the urologists settled with benign diagnoses from MRGB. They then decided to end investigations in these patients.
Purpose
Discrepancy between MRI and TRUS-guided biopsies is a challenge in clinical practice. Despite MRI reported of tumor suspicious lesions, TRUS biopsy will sometimes present benign histology only. Another challenging situation is low-grade prostate cancer proven in the TRUS biopsies while MRI reports suspicion of higher grade cancers. With the implementation of in-bore MR-guided biopsy (MRGB) of the prostate in our hospital we aimed to improve our service for these patients. The purpose of this retrospective study was to evalute if the introduction of MRGB improved the diagnosis of prostate cancer in these patients. We also evaluated to what extent the urologist would trust a benign histology from MRGB.Material and Methods
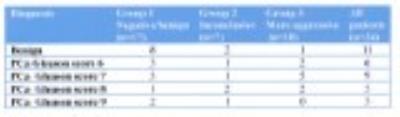
A retrospective journal review of all 34 patients who were referred to MRGB in our hospital from October 2014 to February 2016 was performed, including only patients with MRI showing one or more lesions suspicious of malignancy, and who had been to at least one former TRUS biopsy. The study was approved by the local ethical committee. These patients could be divided into 3 categories according to reasons for referral, as shown in Table 1.
The patients’ mean age was 64 years (57-74), mean PSA 8 ng/ml (3,9-69,4), mean number of repeated TRUS biopsies 2 (1-7). The PI-RADS score of pre-biopsy MRI was 5 in 15 patients, 4 in 18 patients and 3 in 1 patient. The patients were examined and biopsied on a 3T MRI scanner (Siemens Skyra), with a manual biopsy stand (Dynatrim, InVivo). Biopsy needles were MRI compatible, 18G caliber and 175 mm in length. Transrectal approach with the patients in the prone position during biopsy. Lidocain gel for local anestesia. Antibiotic profylaxis. One lesion was biopsied in 27 patients (79%), and 2 lesions in 7 patients (21%). The needle position in the lesion was documented by MRI, as shown in Figure 1.
Results
All of the MR-guided biopsies were of acceptable quality for histologic diagnosis. The diagnoses are shown in Table 2. In the 17 patients with previous negative/benign TRUS biopsies, 9 were upgraded to malignant diagnosis. In the 7 patients with inconclusive histologies a malignant diagnosis was found in 5 and benign in 2. In the 10 patients with MRI-findings suspicious of more aggressive malignancy than proven in TRUS biopsies, 7 were upgraded to intermediate or high grade malignancy, while 1 was benign and 2 were low-grade even by MRGB. For the whole cohort we found high grade cancer (Gleason score 8 or 9) in 8 patients (24%). Seventeen patients there was a Gleason score ≥7 (50%), and when including Gleason score 6 23 patients received a malignant diagnosis (68%). After MRGB the urologists settled with the reported histolgy. For patients with benign diagnoses this lead to an end of investigations. Lowgrade cancer patients, including 1 intermediate grade cancer, were offered active surveillance. The rest of the patients with intermediate and high grade cancers were referred to radical treatment, whereof 11 received robot-assisted radical prostatectomy. Gleason score from MRGB and prostatectomy specimens were identical in 10 patients, while a minimal difference was observed in 1 patient.Discussion
The current study shows the feasibility of MRGB in an ordinary radiologic department with results in the same range as previously reported from a specialized prostate center 1. Our biopsies were considered representative by both pathologists and urologists. Due to the images verifying the position of the biopsy needle inside the MRI lesion, the urologists settled with the diagnosis and implemented treatment and follow-up accordingly. This is important because of the increasing awareness of morbidity related to transrectal biopsies2.Conclusions
In-bore MRGB is a feasible method in an ordinary radiology department.
MRGB is a useful supplement to TRUS biopsy methods because it verifies formerly suspected but undiagnosed cancers .
MRGB improves the care of patients by avoiding unnecessary future biopsies.
Acknowledgements
No acknowledgement found.References
1. Hoeks C M A, Schouten M G, Bomers J G R, et al. Three-Tesla Magnetic Resonance–Guided Prostate Biopsy in Men With Increased Prostate-Specific Antigen and Repeated, Negative, Random, Systematic, Transrectal Ultrasound Biopsies: Detection of Clinically Significant Prostate Cancers. Eur Urol 2012;62:902-909.
2. Lindström K, Drevin L, Carlsson S, et al. Nationwide Population Based Study of Infections after Transrectal Ultrasound Guided Prostate Biopsy. J Urol 2014;192:1116-1122.
Figures