5537
Low-field cardiac MRI for cardiac radiosurgery using an integrated MRI-guided radiotherapy system1Radiation Oncology and Radiology, Washington University in St Louis, St Louis, MO, United States, 2ViewRay, Oakwood Village, OH, United States, 3Radiation Oncology, Washington University in St Louis, St Louis, MO, United States, 4Cardiovascular, Washington University in St Louis, St Louis, MO, United States, 5ViewRay, Mountain View, CA, United States
Synopsis
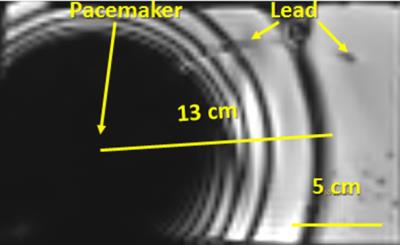
Integrated MRI-guided radiotherapy (MRIgRT) systems perform simultaneous MRI acquisitions during radiation therapy to optimize the accuracy of dose delivery. Cardiac radiosurgery using stereotactic body radiation therapy (SBRT) is a promising new treatment option for cardiac arrhythmias. We imaged the heart with a novel ungated radial TrueFISP sequence on a 0.35 T MRIgRT system. The sequence is being developed for next generation SBRT. Image artifacts associated with the sequence were measured using a Medtronic implantable cardiac defibrillator (ICD) in hydrogel and extended 13 cm from its center. Thus, artifacts should not preclude MRIgRT for most patients with ICDs.
Purpose
Over 325,000 deaths in the US are due to sudden cardiac arrest (SCA), more than lung cancer, breast cancer, and AIDS combined.1 Patients who survive SCA have an estimated 40-60% chance of developing another ventricular arrhythmia in the subsequent year.2 In addition, atrial fibrillation (AF) affects 25% of people aged >40 years.3 Current treatment methods have limited long term success or are not well tolerated (e.g., implantable cardiac defibrillators (ICDs) and medicines for ventricular tachycardia). Cardiac catheter ablation has a five year success of 30% for atrial fibrillation while complications may occur in 5% of patients.
Stereotactic body radiation therapy (SBRT) using image guidance provides a noninvasive option for cardiac radiosurgery. Until recently, image-guided cardiac radiosurgery was performed using either cone-beam CT or biplane x-ray (e.g., Cyberheart).4,5 MRI-guided radiotherapy (MRIgRT) can accurately measure cardiac motion while simultaneously delivering radiation to the targeted location on the heart. In this study, we evaluated fast cardiac MRI acquisitions at low field that are being developed for MRI-guided cardiac radiosurgery.
Methods
Volunteers received cardiac MRI on the ViewRay MRIdian MRIgRT system after providing informed consent. The MRIdian incorporates a 0.35 T MRI running Siemens IDEA/ICE (VB19). The system was equipped with a Physiological Monitoring Unit for gating and monitoring. Volunteers were positioned supine on top of a torso phased array receive coil. A second torso coil was placed on top of the volunteer. Each coil contained 6 receive channels. A respiratory bellows was anteriorly placed on the volunteer to capture respiratory motion. ECG leads were placed on the volunteer’s chest for gating and a peripheral pulse sensor was placed on the finger as a backup.
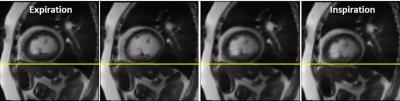
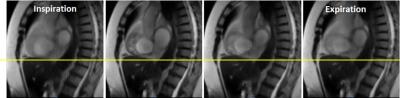
Cardiac MRIs were acquired of the heart using the MRIdian MRI simulation mode. The default MRIgRT protocol uses a three-plane gradient echo localizer, a single breathhold 3D TrueFISP volumetric structural acquisition (1.5 mm in-plane resolution, TE/TR: 1/3 ms, GRAPPA 2, 1000 Hz/pixel, flip angle: 700), and a single-slice 2D sagittal TrueFISP cine (3.5 mm in-plane resolution, TE/TR: 1/2 ms, 2 averages, 0.25 s/image), for motion tracking and gated radiotherapy (RT).
The MRIdian was then placed in the MRI-only mode and operated as a standalone MRI to permit the use of custom pulse sequences. A single-shot radial TrueFISP sequence was used to acquire 2D sagittal cine images of the heart every 0.16 s (TE: 1.34 ms, Matrix: 112, Radial lines: 112, Flip angle: 1100, BW: 893 Hz/pixel). The sequence is being developed for the latest version of radiotherapy (RT) operations, i.e., RT and MRI simulation modes. Real-time iterative reconstruction was implemented in ICE using 8 reconstruction threads and 28 elements/frame. The images were compared with conventional ungated and gated TrueFISP acquisitions.
We also imaged a Medtronic Virtuoso MR Unsafe ICD in hydrogel to assess the extent of artifact since many of the prospective radiosurgery patients have ICDs and TrueFISP is vulnerable to magnetic susceptibilities.
Results
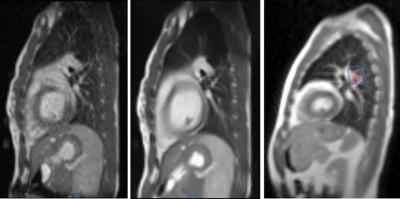
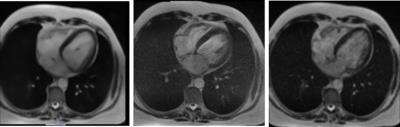
Figure 1 compares the quality of 0.35 T cardiac MRIs for several variants of the TrueFISP sequence including gated and ungated radial acquisitions and a Cartesian acquisition. One of the volunteers had premature ventricular contractions (but no ICD) that did not respond to catheter cardiac ablation treatment (Figs. 2-4). The arrhythmia was successfully captured by the ungated sequences. However, gated acquisitions were unsuccessful due to the severity of the arrhythmia. We noted that the radial TrueFISP sequence caused RF interference with the ECG monitoring.
The image quality and contrast-to-noise ratio at 0.35 T appeared comparable to conventional field strengths. The ICD in hydrogel produced an artifact that extended 13 cm from its center (Fig. 5) thus allowing most patients to be treated on MRI.6
Discussion
This work only addressed the MRI portion of the MRIgRT. The radial TrueFISP sequence was run with a relatively high flip angle (1100) for steady state free precession (SSFP). Such a flip angle would be problematic at higher field strengths due to specific absorption rate limits. SSFP sequences have high contrast-to-noise ratio at low field and are the dominant sequence for cardiac applications.7
Many of the patients with tachycardia have pacemakers or ICDs. Magnetic susceptibility and SSFP artifacts decrease with decreasing magnetic field strength. Hence, low-field can enable MRIgRT procedures that may not be possible at higher fields (e.g., 1.5 T) due to extensive signal dephasing or safety concerns. MR Conditional ICDs are available that will improve safety and potentially reduce artifacts for MRIgRT.
Conclusion
High quality cardiac cine MRIs were successfully acquired at low-field using the radial TrueFISP sequence.Acknowledgements
This research was supported by Washington University in St. Louis’s Department of Radiation Oncology and ViewRay.References
1) Levine GN, et al., 2015 ACC/AHA/SCAI Focused Update on Primary Percutaneous Coronary Intervention for Patients With ST-Elevation Myocardial Infarction: An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and the 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 133(11): 1135-1147 (2016).
2) Fishman GI, et al., Sudden cardiac death prediction and prevention: report from a National Heart, Lung, and Blood Institute and Heart Rhythm Society Workshop. Circulation 122(22):2335-48 (2010).
3) Vroomen M, Pison L. Hybrid ablation for atrial fibrillation: a systematic review. J Interv Card Electrophysiol. Epub ahead of print (2016).
4) Maguire PJ et al., Cardiac Radiosurgery (CyberHeart) for Treatment of Arrhythmia: Physiologic and Histopathologic Correlation in the Porcine Model. Cureus 3(8) e32 (2011).
5) Xia P. et al., A treatment planning study of stereotactic body radiotherapy for atrial fibrillation. Cureus 8(7):e678 (2016).
6) Mesubi O et al., Impact of ICD artifact burden on late gadolinium enhancement cardiac MR imaging in patients undergoing ventricular tachycardia ablation. Pace and Clinical Electrophysiology 37(10): 1274-1283 (2014).
7) Wachowicz K et al., CNR considerations for rapid real-time MRI tumor tracking in radiotherapy hybrid devices: Effects of B0 field strength. Med Physics 43(8): 4903 (2016).
Figures