5493
Real-time frequency and motion corrected Hadamard encoded spectral editing (CHASE)1Danish Research Centre for Magnetic Resonance, Centre for Functional and Diagnostic Imaging and Research, Copenhagen University Hospital Hvidovre, Hvidovre, Denmark, 2Philips Healthcare, Copenhagen, Denmark, 3Dept. Electrical Engineering, Technical University of Denmark, Denmark
Synopsis
Inhibitory neurotransmitter GABA and antioxidant GSH are suggested to be implicated in psychiatric and neurological disorders. These metabolites can be measured in the human brain in vivo using edited 1H-MRS. However, traditional MEGA editing can only be performed for one metabolite at a time, whereas Hadamard encoded spectral editing assesses both metabolites in one sequence, thereby reducing total scan time twofold. As the relatively small GABA and GSH signals as well as the Hadamard paradigm are highly susceptible to frequency drift and motion, real-time frequency and motion correction was added to the sequence.
Purpose
To reduce the time needed to edit multiple small-signal metabolites and correct for frequency drift and motion in real time in the human brain in vivo, resulting in time-efficient and accurate edited 1H-MRS studies.Introduction
The major inhibitory neurotransmitter gamma-aminobutyric acid (GABA) and the dominant antioxidant glutathione (GSH) are both suggested to be implicated in psychiatric disorders, e.g. schizophrenia, depression and autism, and neurological disorders, e.g. Alzheimer’s disease, Parkinson’s disease and Huntington’s disease. Both metabolites can be measured in the human brain in vivo using edited 1H-MRS. However, traditional MEGA editing can only be performed for one metabolite at a time, making the measurement of both metabolites in one study a time-costly exercise.
In MEGA editing1, a refocusing pulse is applied to the coupled resonance in the even acquisitions (edit-on) while in the odd acquisitions J-coupling is not refocused (edit-off). Subtraction of the edit-on and edit-off spectra results in the edited spectrum with a resolved GABA or GSH resonance around 3 ppm.
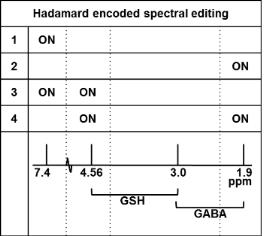
Using a Hadamard scheme2, multiple small-signal metabolites can be simultaneously assessed, resulting in a time-efficient measurement. The method makes use of the fact that although GABA and GSH both have resonances around 3 ppm (3.01 and 2.95 ppm respectively), they have coupled resonances at different frequencies, i.e. 1.89 and 4.56 ppm respectively. Instead of a two-step editing scheme, a four-step Hadamard scheme is applied using a dual band refocusing pulse at 1.9 and 4.56 ppm in the fourth step.
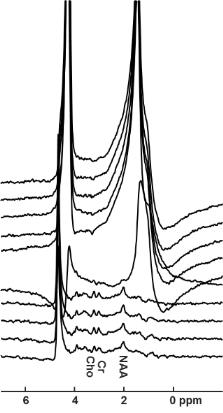
The relatively small GABA and GSH signals as well as the Hadamard paradigm are highly susceptible to frequency drift and motion (Fig.1), although this is usually not clearly visible in the spectrum. Therefore, prospective frequency and motion correction were added to the sequence to update frequency and localization in real time.
Methods
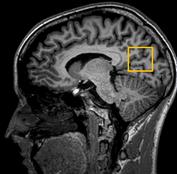
MRS experiments were performed with a 3T MR scanner (Philips, Best, The Netherlands) in combination with a 32-channel receive head coil. Experiments were performed to compare measured GABA and GSH signals between a Hadamard edited PRESS sequence (Fig.2) using frequency and motion correction and the same sequence not using frequency and motion correction (TR/TE=2000/80 ms, 128 averages, 30x30x30 mm3 medial parieto-occipital voxel (Fig.3)) in three healthy subjects. In both instances, subjects were told to move their head halfway through the sequence.
Motion tracking was performed using volumetric 3D EPI navigators3 that were interleaved before water suppression in every MRS acquisition, using a recently developed interleaved scanning framework4. A frequency drift measurement was performed prior to each 3D EPI volume by readouts of the central k-space line. The duration of each navigator and updating module was less than 800 ms.
Measurements were performed according to the local ethical protocols.
Results
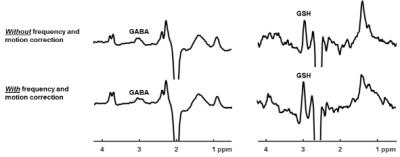
Edited PRESS spectra for parallel GABA and GSH measurement, acquired with and without frequency and motion correction are shown in Fig.4. Although not obvious from the spectra at first glance, the editing scheme was distorted by motion leading to a 25% reduction of the observed GABA signal and a 40% reduction of the observed GSH signal. Motion correction and frequency determination restored full signal intensity.Discussion
Using frequency and motion correction, both the GABA and GSH resonances around 3 ppm are well-resolved and show restored signal intensities as compared to not using frequency and motion correction. Although not always clearly visible in the MR spectrum, frequency and motion correction is essential for accurate assessment of edited metabolites. CHASE allows for time-efficient and accurate assessment of multiple metabolites using just one sequence, therefore making optimal use of the available scan time per subject. The presented data are part of an ongoing study; macromolecule suppression for accurate assessment of the GABA signal will be added to the CHASE paradigm, a test-retest study is planned and CHASE will be implemented at 7T.Acknowledgements
This research is supported by the Danish Council for Independent Research grant no. 6111-00349A.References
1. Mescher M, Merkle H, Kirsch J, Garwood M, Gruetter R. Simultaneous in vivo spectral editing and water suppression. NMR Biomed, 1998, 11:266-272.
2. Saleh MG, Oeltzschner G, Chan KL, Puts NA, Mikkelsen M, Schär M, Harris AD, Edden RA. Simultaneous edited MRS of GABA and glutathione. Neuroimage, 2016, 142:576-582.
3. Tisdall MD, Hess AT, Reuter M, Meintjes EM, Fischl B, Van der Kouwe AJW. Volumetric navigators for prospective motion correction and selective reacquisition in neuroanatomical MRI. Magn Reson Med, 2012, 68:389-399.
4. Henningsson M, Mens G, Koken P, Smink J, Bornar RM. A New framework for interleaved scanning in cardiovascular MR: Application to image-based respiratory motion correction in cornary MR angiography. Magn Reson Med, 2015, 73:692-696.
Figures