5453
Assessment of specific absorption rate and temperature increase induced by artificial hip joints during MRI scans1Korea Research Institute of Standards & Science, Daejeon, Korea, Republic of, 2Medical Physics, University of Science & Technology, Daejeon, Korea, Republic of
Synopsis
Heating of patients or burning of biological tissues by RF power induced by medical implants during MRI scan is a significant patient safety concern. The poor reliability and repeatability of the manufacturer-reported SAR values on clinical MRI systems have been acknowledged. High SAR and temperature change occur on both head and tail of artificial hip joints. It is essential to assess the safety of MRI system for patient with medical implant by measuring not only accurate SAR deposited in the body, but also temperature elevation due to the deposited SAR during clinical MRI.
1404
Purpose: Heating of patients or burning of biological tissues by RF power during MRI scan is a significant patient safety concern. The poor reliability and repeatability of the manufacturer-reported SAR values on clinical MRI systems have been acknowledged1,2. The purpose of this study is to not only measure SAR values, but also RF-induced temperature elevation due to artificial hip joints at 1.5 and 3T MRI systems.
Methods: SAR measurement experiment was performed on three discrete manufacturers at 1.5 and 3T (one 1.5T and two 3T MRI scanners) using a 2-channel volume transmit coil and a 4-or 8-channel torso receive coil. Three MRI RF sequences (T1w TSE, T2w inversion recovery, and T2w TSE) with imaging parameters were selected. According to American Society for Testing and Materials (ASTM) F2182-11a, a hydroxyl-ethylcelluose (HEC) gelled saline phantom (14 L) mimicking human body tissue was made. Human body phantom were constructed, based on Korean adult standard anthropometric reference data (Fig.1). The finite difference time domain (FDTD) method was utilized to calculate the SAR distribution using CST studio suite 2014 (CST Computer Simulation Technology Co.). The number of simulation mesh cells were 221,108 and the mesh cell ratio is 0.8~2.2. Based on the results of the simulation, 4 electrical field (E-field) sensors were located around two artificial hip joints inside the phantom. 56 Fiber Bragg Grating (FBG) temperature sensors (28 sensors on each artificial hip joint) were located on both left and right artificial hip joints to measure temperature change during MRI scan (Fig.1). Both E-field and FBG temperature sensors were calibrated with traceability at Korea Research Institute of Standards and Science (KRISS).
Results: Simulation shows that high SAR values occur in the head and tail of the implanted artificial hip joints (Fig.1 lower right). One 1.5T and one of two 3T MRI systems represent that the measured SAR values were lower than MRI scanner-reported SAR values. However, the other 3T MRI scanner shows that the averaged SAR values measured by probe 1, 2, and 3 are 2.30, 2.77, and 1.68 W/kg, compared to MRI scanner-reported whole body SAR value (≤1.5 W/kg) for T1w TSE and T2w_IR (Table 1). The maximum temperature elevation measured by FBG sensors is 1.49°C at 1.5 T, 2.0°C at 3 T, and 2.56°C at Discussion: High SAR and temperature change occur on both head and tail of artificial hip joints. The averaged SAR values measured in probe 1, 2, and 3 at 3 T are higher than MRI scanner-reported whole body SAR value and lower than SAR limit(=4W/kg) required by IEC(International Electrotechnical Commission) 60601-2-33 for T1w TSE and T2w_IR. However, temperature elevation on the tail of the implant artificial hip joints for T1w TSE at 3 T are higher than the limits for temperature required by IEC 60601-2-33 (Table 201.104).
Conclusion: It is essential to assess the safety of MRI system for patient with medical implant by measuring not only accurate SAR deposited in the body, but also temperature elevation due to the deposited SAR during clinical MRI.3 T for T1w TSE, respectively (Table 2).
Acknowledgements
No acknowledgement found.References
[1] Seo et al. RF dosimeter for the measurement of specific absorption rate (SAR) in MRI, RSNA 98th scientific assembly and annual meeting, Chicago, Illinois, Nov.25-30, 2012
[2] Seo et al. Evaluation of MRI scanner-reported specific absorption rate values and measurement of temperature change during MRI scan at 3 T, RSNA 100th scientific assembly and annual meeting, Chicago, Illinois, Nov.30-Dec.5, 2014
Figures
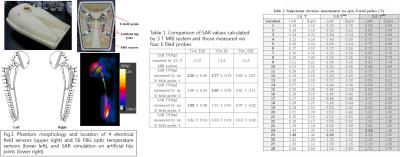
Fig.1 Phantom morphology and location of 4 electrical field sensors and 56 optic temperature sensors, and SAR simulation on artificial hip joints.
Table 1. Comparison of SAR values callculated by 3 T MRI system and those measured via 4 E-field sensor
Table 2. Temperature elevation measurement via 4 optic temperature sensors