5394
The Combine Analysis of improved Multi-parametric MR for identifying the different subtypes and immunohistochemical expression of Breast cancer1Department of Radiology(MRI), Meizhou City People's Hospital, Meizhou,Guangdong, People's Republic of China, 2Department of Radiology(MRI), Meizhou City People's Hospital, People's Republic of China, 3Department of breast surgery, Meizhou City People's Hospital, Meizhou,Guangdong, People's Republic of China, 4Departmen of Siemens Healthcare application, Siemens Healthcare, Guangdong, People's Republic of China, 5MR scientific marketing NE Asia, Siemens Healthcare, Guangdong, People's Republic of China, 6MR scientific marketing NE Asia, Siemens Healthcare, Beijing, People's Republic of China
Synopsis
The aim of this study was to explore the different subtypes and immunohistochemical expression of breast cancer in improved multi-parametric MR imaging. By introducing the free breathing of ultrafast temporal resolution dynamic VIBE (TWIST-VIBE) and readout segmentation of long variable echo-trains (RESOLVE) techniques, quantitative pharmacokinetic (PK), semi-quantitative DCE-MRI based on curve of time concentration and diffusion parameters were extracted to analyze it. The results show that significant differences in multi parametric parameters Kep and rADC among the different subtypes of Breast cancer. Those parameters were hopeful to be a non-invasive measurement for assessing the subtypes and the biology, histological features of breast cancer.
Introduction and purpose
Histopathology is the golden standard for diagnosing the different subtypes of breast cancer, but it’s traumatic for patients. Different biological and histological features of breast cancer appear as different morphological and functional characteristics on MRI.1,2 The time-resolved angiography with interleaved stochastic trajectories (TWIST) technology was a prototype sequence, which was available for high temporal resolution quantitative and semi-quantitative dynamic contrast-enhanced (DCE). Readout segmentation of long variable echo-trains diffusion weighted imaging (RESOLVE-DWI) sequence was combined to analyze the different expression of subtype breast cancer. The purpose of this study was to explore the differential diagnosis significance of multi-parametric MRI in the different subtypes and immunohistochemical expression of Breast cancer.Methods
Totally 69 female patients (mean age 49.9 ± 1.5 years, range 25 - 79 years) with proved breast cancer underwent breast MRI scanning on a 3T MRI scanner (Magnetom Skyra, Siemens Healthcare, Erlangen, Germany) with (16-channel phased-array breast coil, prone position, head enter firstly), A prototype TWIST-VIBE sequence as follow: TR/TE = 6.4/3.3 ms, FA = 9.0, 288 mm × 384 mm FOV, 2 mm slice thickness without slice gap, 34 phases as first phase = 17.7 s and later phase = 8.7 s per phase within 5 min 5 s, following intravenous injection of 0.2 ml/kg of gadopentetate dimeglumine, a RESOLVE-DWI sequence with 2 b values (50, 800 s/mm2), TR/TE = 4800/56 ms, FA = 180, 170 mm × 340 mm FOV, 4 mm slice thickness with 0.8 slice gap, a common EPI-DWI sequence with 3 b values (50, 400, 800 s/mm2) , TR/TE = 4200/62 ms, 149 mm × 340 mm FOV, 4 mm slice thickness with 0.8 slice gap, and the routine T2WI, T1WI sequences were performed. [2] All the imagines analysis and processing were carried out by two attending radiologist with more than 5 years working experience. The PK model and the semi-quantitative model were used to co-analyze the patients respectively. Data analysis: All the value (including the quantitative PK parameters, semi-quantitative parameters and ADC) were measured as ROI drawn within the tumor lesion avoiding the blood vessel. The parametric maps are all obtained by using the Syno. Via platform (Siemens Healthcare, Erlangen, Germany). Immunohistochemical technique were introduced to classify the different molecular subtypes of breast cancer.3 Combining statistic of multiple parameters were analyzed by SPSS as those subtypes classification of breast cancer.Results
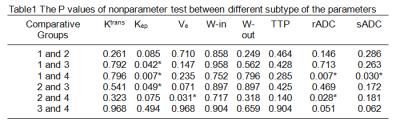
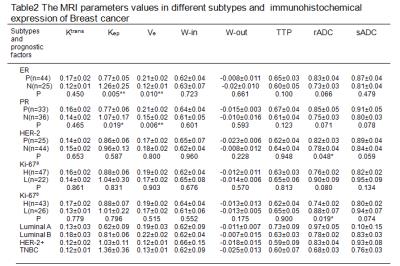
High temporal resolution images and parametric maps with time-concentration curve were obtained. (Figure 1). In these 69 cases, Luminal A, Luminal B, HER-2, TNBC was 12, 34, 8, 15 cases respectively. There were statistically significant difference of Kep, rADC values between different molecular subtypes (P = 0.014, 0.023 respectively), Kep was highest in TNBC type and lowest in Luminal A type, rADC values was highest in Luminal A type and lowest in TNBC type. Kep show significant difference between Luminal A and HER-2, Luminal A and TNBC, Luminal B and HER-2; rADC values show significant difference between Luminal A and TNBC, Luminal B and TNBC; and also there were significant difference of Ve between Luminal B and TNBC (P = 0.031). Meanwhile, of sADC values between Luminal A and TNBC (P = 0.030) (Table1). Kep values were significantly higher and Ve values were significantly lower in the ER, PR-negative compared to the ER, PR-positive, rADC values were significantly lower in the HER-2-negative compared to the HER-2-positive (P = 0.048) (Table2). And there’s low correlation between the Kep, Ve values and the ER expression(P = 0.004, 0.009 and r = 0.353, 0.324 respectively), meanwhile between the Ve values and the PR expression(P = 0.005, r = 0.351). All of these MRI parameters show no significant difference between high(expression ≥ 14%) and low expression(expression < 14%) of Ki-67, but rADC values were significantly lower when Ki-67 positive expression ≥ 20% compared to Ki-67 positive expression < 20% (P = 0.019) (Table2).Discussion and Conclusion
The PK and semi-quantitative parameters in DCE-MRI and the rADC values in readout segementation EPI diffusion show significant difference between different subtypes. High Kep value and low Ve value suggest possible ER, PR-negative, low rADC value may indicate HER-2 low expression and Ki-67 high expression, it’s possible TNBC subtype with high Kep value and lower rADC value, and it’s possible Luminal A subtype with low Kep value and high rADC value. These results proved that the Kep, Ve, rADC values could reflect the biological and histological characteristics of breast cancer partly, and they were hopefull to be non-invasive indicators for evaluating the subtypes and the biology, histologic features of breast cancer
Acknowledgements
No acknowledgement found.References
No reference found.Figures