5278
Shared and Specific Intrinsic Functional Connectivity Patterns in Unmedicated Bipolar Disorder and Major Depressive DisorderYing Wang1, Junjing Wang2, Yanbin Jia3, Tao Liu3, Yao Sun1, Shuming Zhong3, Zhongping Zhang4, Li Huang1, and Ruiwang Huang2
1Medical Imaging Center, First Affiliated Hospital of Jinan University, Guangzhou, People's Republic of China, 2Center for the Study of Applied Psychology & MRI Center,Center, Key Laboratory of Mental Health and Cognitive Science of Guangdong Province, School of Psychology, South China Normal University, Guangzhou, 3Department of Psychiatry, First Affiliated Hospital of Jinan University, Guangzhou, People's Republic of China, 4MR Research China, GE Healthcare, Beijing
Synopsis
Our findings suggest that bipolar disorder (BD) and major depressive disorder (MDD) may have some shared and morespecific impairments of functional connectivity patterns during the depressiveperiod, providing new evidence for pathophysiology of BD and MDD at thelarge-scale whole brain connectivity level.
Introduction
Identification of brain structural and functional differences and similarities between bipolar disorder (BD) and major depressive disorder (MDD) is a necessary step to better understand the pathophysiology of affective disorders and develop more effective treatments. However, the features of whole-brain intrinsic functional connectivity underlying BD and MDD have not been directly compared.Methods
We collected resting-state functional magnetic resonance imaging data from 55 depressive BD patients, 52 MDD patients, and 52 healthy subjects. MRI scans were performed on a 3.0T whole-body scanner (Discovery 750, GE Medical System, Milwaukee, WI). The clinical state for each patient was assessed using the 24-item Hamilton Depression Rating Scale (HDRS) and the Young Mania Rating Scale (YMRS). We constructed voxel-wise whole-brain functional networks and computed regional functional connectivity strength (FCS) using graph-theory, and further divided regional FCS into long-range FCS (lFCS) and short-range FCS(sFCS).Results and Discussion
Relative to the healthy control group, both MDD and BD patients showed decreased lFCS and sFCS in the bilateral precuneus, but increased sFCS in the bilateral calcarine. The MDD patients showed decreased lFCS in the cerebellum compared to the controls and BD patients. Whereas the BD patients showed more widespread abnormal lFCS and sFCS in regions of the cerebello-thalamo-prefrontal pathway, including the bilateral thalami, leftsuperior frontal gyrus, bilateral medial frontal gyri, and cerebellum, andincreased lFCS in the left superior temporal gyrus and right middle temporalgyrus. In addition, for the BD patients, the lFCS of the bilateral medial frontal gyri and right superior temporal gyrus were positively correlated with total HDRS scores; the lFCS of the bilateral medial frontal gyri was positively correlated with the number of episodes. While for the MDD patients, no significant correlation was found between the FCS and any of clinical variables.Conclusion
The findings suggest that BD and MDD may have some shared and more specific impairments of functional connectivity patterns during the depressive period, providing new evidence for pathophysiology of BD and MDD at the large-scale whole brain connectivity level.Acknowledgements
No acknowledgement found.References
No reference found.Figures

Statistical results in the lFCS among BD, MDD and healthy controls.(a) Clusters showing significant group effects (p < 0.05 Alphasim corrected,ACNOVA). (b) Post-hoc analyses of lFCS for these significant clusters. The ‘BD’ type indicates that the lFCS in the cluster was altered specific to the BD but not to the MDD. The ‘shared’ type indicates that the cluster with altered lFCS was detected in both the BD and MDD. Abbreviations: lFCS, long-range functional connectivity strength; BD (MDD),bipolar (major depressive) disorder; STG, superior temporal gyrus; MTG,middle temporal gyrus; MFG, medial frontal gyrus
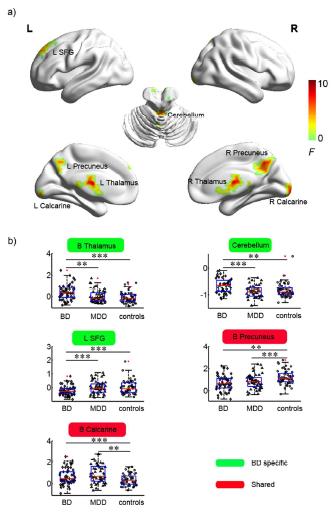
Statistical results in the sFCS among BD, MDD and healthy controls.(a) Clusters showing significant group effects (p < 0.05 Alphasim corrected,ACNOVA). (b) Post-hoc analyses of sFCS for the significant clusters. The ‘BD’ type indicates that the sFCS in the cluster was altered specific to the BD but not to the MDD. The ‘shared’ type indicates that the cluster with altered sFCS was detected in both the BD and MDD. Abbreviations: sFCS, short-range functional connectivity strength; BD (MDD),bipolar (major depressive) disorder; SFG, superior frontal gyrus.
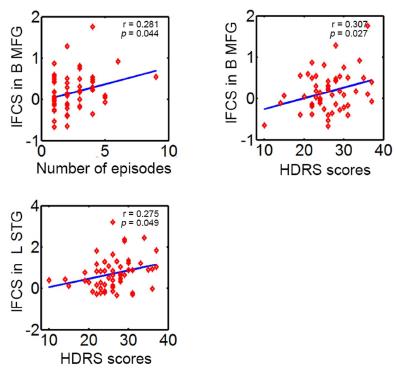
Relationship between the lFCS and clinical variables in the BD group.The lFCS value of bilateral MFG was significantly positive correlated with the number of episodes (r = 0.281, p = 0.044). In addition, the lFCS values of bilateral MFG and left STG were significantly positive correlated with the HDRS scores, respectively (MFG: r = 0.307, p = 0.027; STG: r = 0.275, p =0.049). The symbol of ◊ indicates a subject in the BD group. Abbreviations:lFCS, long-range functional connectivity strength; BD, bipolar disorder; MFG,medial frontal gyrus; STG, superior temporal gyrus; HDRS, the HamiltonDepression Rating Scale; B (L), bilateral (left).