5191
Accurate and reliable fat-water MRI breast density measurements1Biomedical Engineering, Stony Brook University, Stony Brook, NY, United States, 2Pathology, Stony Brook Medicine, Stony Brook, NY, United States, 3Cancer Center, Stony Brook Medicine, Stony Brook, NY, United States, 4Biomedical Informatics, Stony Brook Medicine, Stony Brook, NY, United States, 5Computer Science, Stony Brook University, Stony Brook, NY, United States, 6Cancer Center, University of Arizona, Tucson, AZ, United States, 7Medical Imaging, University of Arizona, Tucson, AZ, United States, 8Epidemiology and Biostatistics, University of Arizona, Tucson, AZ, United States, 9Stony Brook Medicine, Stony Brook, NY, United States, 10Cancer Center, University of Hawaii at Manoa, Honolulu, HI, United States, 11Hematology and Oncology, Stony Brook Medicine, Stony Brook, NY, United States, 12Radiology, Stony Brook Medicine, Stony Brook, NY, United States, 13Psychiatry, Stony Brook Medicine, Stony Brook, NY, United States
Synopsis
Breast density (BD) is a risk factor for breast cancer, which makes the accurate measurement of BD a priority. Mammography is most widely used for BD determination (MG-BD) but ionizing radiation prohibits its use. BD derived from fat-water decomposition MRI (FWMRI-BD) has been proposed. Here we developed an optimized FWMRI-BD measurement (FraG+W) and compared it to MG-BD and a previous FWMRI-BD measurement (Fra80/90). Both FWMRI-BD measures were strongly correlated with MG-BD and exhibited superior test-retest reliability. The proposed automated FraG+W, which quantifies the entire fibroglandular and water content of the breast, is more accurate and reliable than the previous Fra80/90.
Purpose
Breast density (BD) is a radiologic or image based measure of the proportion of fat to glandular and fibrous tissues in the breast where higher BD is a risk factor for breast cancer 1. High BD also limits tumor detectability by mammography. As such, the accurate measurement of BD has emerged as a priority for assessing breast cancer risk and as part of the interpretation of mammographic findings. Currently, mammography is the most widely used method of BD determination (MG-BD) but the requirement for ionizing radiation prohibits its use in studies requiring frequent monitoring. BD derived from fat-water decomposition MRI (FWMRI-BD) has been proposed 2 as an alternative for BD quantification without ionizing radiation. We developed an optimized FWMRI-BD measurement that is automated, more accurate and reliable. In this study, we compare our new method to MG-BD and a FWMRI-BD measurement reported previously.Methods
The study population included two subsets of pre- and post-menopausal women receiving tamoxifen therapy for early stage breast cancer or as primary chemoprevention. The majority of MRI scans were performed on a 1.5T GE Signa NV-CV/i scanner using an axial radial gradient and spin-echo pulse sequence 3. The remaining MRI scans were performed on a 3T Siemens Skyra using an axial Cartesian 6-echo gradient echo pulse sequence. The total acquisition time was <5 min for both sequences and quantitative fat fraction maps of the entire breast volume were generated. A validated automated breast segmentation 4 was applied to all scans. For the enrolled participants who had prior early stage breast cancer, only data from the contralateral unaffected breasts were analyzed. FWMRI-BD was initially calculated using a previous published measure Fra80 2 for data collected on the GE scanner, which represents the ratio of breast voxels with <80% apparent fat fraction. For data collected on the Siemens scanner, due to scanner hardware and acquisition sequence differences, Fra90 was found to be most comparable to Fra80 from the GE scanner.
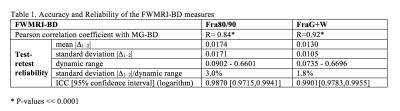
Here we propose a new FWMRI-BD measure, FraG+W. This measure accounts for the total amount of fibroglandular tissue (FraG) and water content (FraW) in the breast, which also mathematically corrects for fat-water signal intensity bias and fat-water signal shine-through due to intrinsic limitation of the chemical shift difference based fat water separation technique. To test the accuracy of FWMRI-BD, MG-BD was used as the gold standard as it is currently the most accepted measure of BD. For this study, 50 patients (mean age ± std: 54.9 ± 8.2 years) undergoing digital MG within 6 months from the date of MRI scan (42 patients from the GE scanner, 8 from the Siemens scanner) were identified and MG-BD was assessed using a well-established quantitative method (Cumulus) 5. Pearson correlation analysis was performed to compare MG-BD and FWMRI-BD. To test the reliability of FWMRI-BD, 26 repeated scans (24 from the GE scanner, 2 from the Siemens scanner) from 10 patients (mean age ± std: 56.4 ± 10.4 years) were identified. For each repeated scan, the patient completely left the scanner and was repositioned in the scanner, re-registered and re-localized. The |∆1–2| values were calculated as the absolute difference between test-retest FWMRI-BD. Test-retest reliability was evaluated using the mean and standard deviation of |∆1–2| and intra-class correlation (ICC) 6 analysis in Matlab.
Results
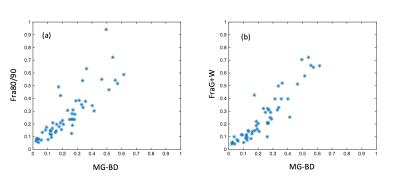
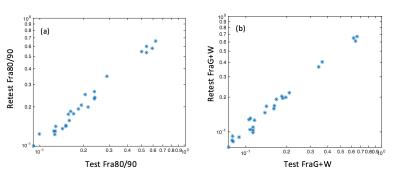
Derived from a representative breast slice collected on the GE scanner, the fat fraction map, the corresponding Fra80 mask, FraG mask, and corrected FraW map are shown in Figure 1(a)-(d). Figure 2 illustrates the correlation between MG-BD and FWMRI-BD (Fra80/90 and FraG+W respectively) and Figure 3 demonstrates the test-retest reliability of Fra80/90 and FraG+W. All statistical analyses are shown in Table 1. Both FWMRI-BD measures were strongly correlated with MG-BD and showed high test-retest reliability (ICC>0.98) compared to MG-BD values from the literature (reported intrareader ICC range 0.82-0.97) 7. FraG+W showed improvement over Fra80/90 in all measures tested.Conclusion
Both FWMRI-BD measures (Fra80/90 and FraG+W) were strongly correlated with MG-BD and exhibited superior test-retest reliability. The proposed automated FraG+W measure, which quantifies the entire fibroglandular and water content of the breast, is more accurate and reliable than the previous FWMRI-BD method. This enables the possibility of early detection of individual BD changes for clinical trials and individual treatment response assessment.Acknowledgements
NIH grants CA149417, CA161534.References
1. McCormack VA, dos Santos Silva I. Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiology Biomarkers & Prevention. 2006;15(6):1159-1169.
2. Thomson CA, Thompson PA, Wertheim BC, Roe D, Marron MT, Galons J-P, Kupinski MA, Altbach MI, Maskarinec G, Stopeck A. Abstract P6-01-18: 2-Hydroxyestrone is associated with breast density measured by mammography and fat: water ratio magnetic resonance imaging in women taking tamoxifen. Cancer Research. 2015;75(9 Supplement):P6-01-18-P06-01-18.
3. Huang C, Altbach MI. Multi-Mask Multi-Seed Free Growing Field Map Estimation Algorithm for Iterative Multi-Point Water-Fat Decomposition. Paper presented at: ISMRM 17th Annual Scientific Meeting & Exhibition, 2009; Honolulu, Hawaii, USA.
4. Ding J, Thompson PA, Marron MT, Altbach MI, Roe D, Galons J-P, Thomson CA, Wang F, Stopeck A, and Huang C. The test-retest reliability of fat-water ratio MRI derived breast density measurements and automated breast segmentation. Paper presented at: ISMRM 24th Annual Scientific Meeting & Exhibition, 2016; Singapore.
5. Byng JW, Yaffe MJ, Jong RA, Shumak RS, Lockwood GA, Tritchler DL, Boyd NF. Analysis of mammographic density and breast cancer risk from digitized mammograms. Radiographics. 1998;18(6):1587-1598.
6. McGraw KO, Wong SP. Forming inferences about some intraclass correlation coefficients. Psychological methods. 1996;1(1):30.
7. Haars G, van Noord PA, van Gils CH, Grobbee DE, Peeters PH. Measurements of breast density: no ratio for a ratio. Cancer Epidemiology Biomarkers & Prevention. 2005;14(11):2634-2640.
Figures