5147
Dynamic susceptibility contrast perfusion MR imaging in distinguishing malignant from benign soft tissue tumors in limbs: A pilot study1Fisrt Affiliated Hospital of Xi'an Jiaotong University, Xian, People's Republic of China, 2General Affiliated Hospital of Ningxia Medical University, Yinchuan, People's Republic of China, 3Luoyang Central Hospital Affiliated to Zhengzhou University
Synopsis
Precise differential and qualitative diagnoses for extremities soft tissue tumors(STTs) are of vital importance. Dynamic susceptibility contrast perfusion MRI(DSC-MRI) enables assessment of overall tumor vascularity, allowing indirect evaluation of the biological aggressiveness of tumors. Therefore, this study aims to discuss the feasibility of DSC-MRI to preliminarily assess in the differentiation between benign and malignant extremities STTs. Our results showed that DSC-MRI might be a non-invasive imaging technique that can play a role in identifying malignant and benign STTs in limbs and provide reliably pathological or physiological information for clinic.
Introduction
Soft tissue tumors(STTs), with low incidence and diagnose rate, are characterized with wide variety and heterogeneity. Therefore, precise differential and qualitative diagnoses are of vital importance for tumor’s treatment strategies and prognosis. The morphology of STTs in regular magnetic resonance imaging(MRI) cannot be distinguished qualitatively between benign and malignant lesions. While the dynamic susceptibility contrast MRI(DSC-MRI), an intravenously administered bolus of contrast agent passes through the intravascular space, which creates local magnetic susceptibility (T2*) effects resulting in signal drop during the first pass of the contrast agent. Studies have showed that DSC-MRI enables assessment of overall tumor vascularity, allowing indirect evaluation of the biological aggressiveness of tumors. To our knowledge, the predictive value of DSC-MRI in patients with STTs has not been investigated yet. Therefore, this study aims to discuss whether DSC-MRI can be used as a biomarker to preliminarily assess the feasibility of DSC-MRI in the differentiation between benign and malignant STTs, and to analyze the best judgement of perfusion parameters.Methods
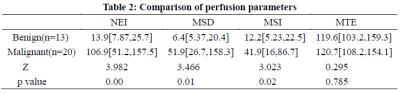
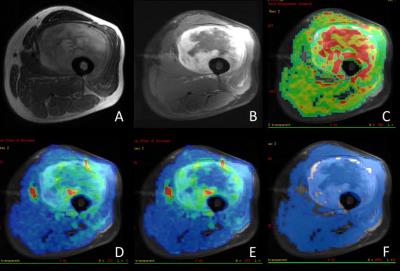
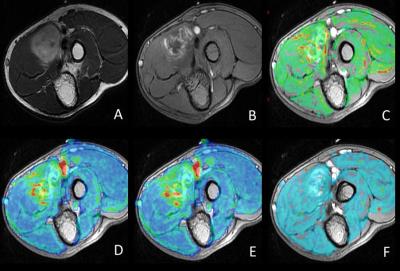
A prospective study was done among 33 patients (16 males and 17 females) with STTs in limbs who underwent DSC T2*-weighted perfusion MRI after bolus infusion of gadolinium-DTPA. The signal intensity time curve of the lesion was created and several certain semi-quantitative parameters were analyzed, including negative enhancement integral(NEI),maximum slope of decrease(MSD), maximum slope of increase(MSI), and mean time to enhance(MTE).NEI represents the relative vascular volume (rBV) of organizational unit volume, MSD and MSI represents respectively TIC maximum signal loss during the descending and ascending scanning segment, which is on behalf of micro-circulatory relative blood flow (rBF). MTE represents the time that the contrast agents go through the organization, which reflect the vascular resistance.Discriminant analyses were performed to reveal parametric differences of benign and malignant lesions. Receiver operating characteristic (ROC) analysis was used to assess the diagnostic efficiency of parameters. All statistical analysis were performed by using SPSS 17.0 (SPSS, Chicago, IL, USA); p<0.05 was considered as statistically significant difference.Results
Diagnosis of benign (N=13) tumors were Hemangioma(n=4), Lipoma(n=4), Neurilemmoma(n=1), Neurofibroma(n=1), Non-ossifying fibroma(n=2), Giant cell tumor of tendon sheath granuloma(n=1), whereas malignant lesions (N=20) were classified as Liposarcoma(n=5), Fibrosarcoma(n=5), Undifferentiated pleomorphie sarcoma(n=2), Malignant myofibroblastoma(n=1), Malignant melanoma(n=2), Non-Hodgkin lymphoma(n=2), Synovial sarcoma(n=2), Alveolar soft part sarcoma(n=1). Several parameters of perfusion (NEI, MSD, MSI) were significant differences between benign and malignant tumors. But MTE parameter was no significant difference in terms of statistics. The area under the curve (AUC) of NEI, MSD, MSI was 0.915, 0.862, 0.815 respectively. The diagnostic efficiency of NEI was highest for differentiating benign from malignancy in STTs and the sensitivity, specificity, accuracy and positive/negative predictive value(PPV/NPV) were 100%,84.6%,93.9%,90.9% and 100% respectively.Discussion
In our study, we used this method by analyzing the signal intensity variations in order to create colorimetric maps, without adopting the arterial input. ROIs placement was basically designed on the enhanced substantial component of tumor’s edge according to the theory of different enhancement of edge and center, which reflected the turevascularization of tumor and avoid ingnecrosis, cystic and hemorrhage. Our results showed that there were significant differences between benign and malignant groups in NEI, MSD and MSI. The reason is that malignant tumor has a high micro-vessel density, the abnormality of cell structure and the incomplete basement, it results in a higher blood flow of microcirculation, higher relative blood volume compared the benign tumor. The MTE performance of benign and malignant tumors had overlap and no significant difference. It illustrates that the enhanced time of tumor has no relationship with perfusion of contrast agent. MTE cannot be applied in the diagnosis of benign and malignant tumors. However, the reliability of parameters in evaluating the tumor microcirculation needs further study.Conclusion
DSC-MRI might be a non-invasive imaging technique that can play a role in identifying malignant and benign STTs in limbs and provide reliably pathological or physiological information for clinic.Acknowledgements
No acknowledgement found.References
1. Noebauer-Huhmann, I.M., et al., Use of diagnostic dynamic contrast-enhanced (DCE)-MRI for targeting of soft tissue tumour biopsies at 3T: preliminary results. Eur Radiol, 2015. 25(7): p. 2041-8.
2. Oliveira, A.M. and A.G. Nascimento, Grading in soft tissue tumors: principles and problems. Skeletal Radiol, 2001. 30(10): p. 543-59.
3. Drape, J.L., Advances in magnetic resonance imaging of musculoskeletal tumours. Orthop Traumatol Surg Res, 2013. 99(1 Suppl): p. S115-23.
4. Nguyen, T.B., et al., Comparison of the Diagnostic Accuracy of DSC- and Dynamic Contrast-Enhanced MRI in the Preoperative Grading of Astrocytomas. AJNR Am J Neuroradiol, 2015. 36(11): p. 2017-22.
Figures