5134
Dynamic Morphometric Changes in Degenerative Lumbar Spondylolisthesis: A Pilot Study of Standing Magnetic Resonance Imaging1Department of Orthopaedics, Centre Hospitalier Universitaire de Québec, Quebec, QC, Canada, 2Department of Orthopaedics, University of British Columbia, Vancouver, BC, Canada, 3Department of Orthopaedics, University of British Columbia, 4Center for Hip Health and Mobility, University of British Columbia, 5Department of Radiology, Vancouver General Hospital
Synopsis
The planning of spine surgery for degenerative lumbar spondylolisthesis (DLS) is currently based on supine MR images while patients experience symptoms in the upright posture. This study employed an upright Open MRI to determine whether the MRI-based measurements of the spinal and neural elements used in planning surgery are different in the symptomatic, upright posture than in the supine posture. We found upright MRI scanning detected dynamic morphometric differences in a number of clinically important radiographic parameters in patients with DLS. Upright MRI may help in planning minimally invasive surgeries for DLS.
INTRODUCTION
Degenerative lumbar spondylolisthesis (DLS), which results in neural compression, pain and weakness, is one of the most common indications for spine surgery. Patients experience symptoms in the upright posture, which are relieved with lying down. Generally, DLS involves a vertebral body slip as a result of degeneration, but DLS presents with a wide spectrum of discrete pathologies, with a wide range of treatments. There is recent interest in ‘anatomy sparing’ surgical approaches that minimize the surgical dissection and thus complications. A limitation to anatomy sparing approaches is that surgical planning is currently based on supine MR images, which do not allow visualization of the neural elements or the tissues to be surgically removed in the symptomatic upright posture.PURPOSE
The objective of this study was to determine whether the MRI-based measurements of the spinal and neural elements used in planning surgery are different in the symptomatic, upright posture than in the supine posture.METHODS
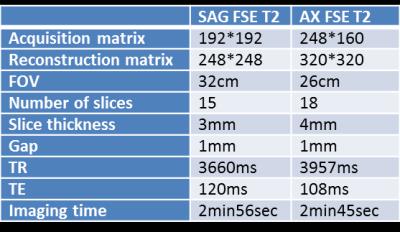
Patients with DLS were scanned upright and supine in a 0.5T upright open MR scanner (MROpen, Paramed, Genoa Italy), as shown in Figure 1(a). Ethics approval was obtained from our institution. Patients with single level, Grade I or II L4/5 DLS, on the surgical waitlist at a single institution, were consented to participate. An imaging protocol was developed with a group of healthy volunteers (n=15). With both upright and supine postures, we acquired images using T2 weighted Fast Spin Echo (FSE T2) sequences in both sagittal and axial planes (Table 1).
We positioned the patient with the L4-L5 disc at the scanner isocentre during imaging. For upright scans, as shown in Figure 1(b), participants stood as upright as possible. Two extension bars were tightened behind the participant when in the upright position to minimize back and forth sway. Foam pads were also placed at both side of the hips to prevent swaying left and right. Another extension bar located at the front of the participant supported the hand and the arm. A pump and pressure cuff system on both legs was used to maintain blood circulation and minimize the risk of loss of consciousness.
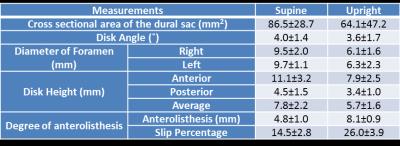
We made the following established measures of the spinal and neural elements, using established protocols: cross sectional area of the dural sac, disc angle, diameter of foramen, disc height, and degree of anterolisthesis. We compared measures from supine and upright images using paired t-tests.
RESULTS
Eight patients (aged 54-73 with a mean age of 65 years) with DLS were included, 5 of which were female. The central slices of SAG scan in both upright and supine postures were shown in Figure 2. The mean and standard deviation of the measurements were listed in Table 2.
Patients scanned in the upright position had reliably measureable and significantly lower cross sectional area of the dural sac (p<0.01), disc height (p<0.001), and both left and right mid foramen diameter (p<0.001) than on supine imaging. The change in absolute slip percentage was found to be 5.5% in Grade I DLS (n=5, p=0.0638), and 13.7% in Grade II DLS (n=5, p<0.0001). The magnitude of change in disc angle was the same for both Grade I and II DLS.
DISCUSSION
In this pilot study, imaging in the symptomatic, upright posture showed smaller disc height, cross sectional area and mid foramen diameter than in the supine position.
The changes from supine to upright posture are not surprising given that the upright posture applies larger loads to the vertebrae and changes their relative position. The observed changes are consistent with the finding that DLS symptoms are experienced in the upright posture. We observed changes in DLS patients from supine to upright that were not seen in a study performed on healthy athletes in supine and upright MRI(1), which is likely due to the instability characterizing DLS.
The key strength of upright MRI to assess DLS is that it allows direct visualization of the relationships between spinal and neural elements. A substantial limitation is that holding a stable standing position is challenging for DLS patients, which makes it difficult to reduce motion artefact. However, this can be addressed with careful patient instruction and adequate support padding.
CONCLUSION
Upright MRI scanning detected dynamic morphometric differences in a number of clinically important radiographic parameters in patients with DLS. Upright MRI may help in planning minimally invasive surgeries for DLS.Acknowledgements
No acknowledgement found.References
1. Mauch F, Jung C, Huth J, Bauer G. Changes in the lumbar spine of athletes from supine to the true-standing position in magnetic resonance imaging. Spine (Phila Pa 1976). 2010;35(9):1002–7.Figures