5127
Evaluation of T1p time in the quadriceps muscle after an Anterior Cruciate Ligament Reconstruction: Relationship to muscle strength and injury recovery1Rehabilitation Sciences, University of Kentucky, Lexington, KY, United States, 2Orthopaedic Surgery, University of Kentucky, Lexington, KY, United States, 3University of Kentucky, Lexington, KY, United States, 4Radiology, University of Kentucky, Lexington, KY, United States, 5Department of Physiology, University of Kentucky, Lexington, KY, United States, 6Department of Bioengineering, University of California Berkeley, CA, United States
Synopsis
Anterior Cruciate Ligament Injuries are associated with long term loss of quadriceps muscle strength. Accumulation of greater collagen in the extracellular matrix around muscle fibers could limit recovery. T1p applied to the quadriceps muscle could identify patients at risk for not having a good recovery because of collagen deposition. T1p imagining of the injured and non injured quadriceps of 6 subjects was performed. We found significantly higher T1p times in the injured limb as well as a significant association to greater muscle weakness. These results show the potential application of T1p to identify individuals with muscle dysfunction.
Introduction
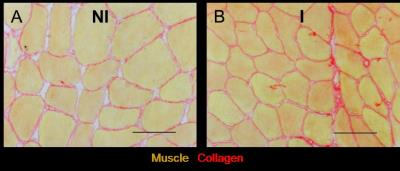
Over 250,000 individuals suffer an anterior cruciate ligament (ACL) tear of the knee in the United States annually 1-3. The injury and subsequent surgery results in profound weakness of the quadriceps muscle. Regaining strength of the quadriceps is critical to provide stability to the knee joint and stabilize the knee4,5 6 7,8. Despite physical therapy patients struggle to regain quadriceps muscle strength which is directly related to negative short and long term outcomes 4,5 6 7,8. We have previously shown following an ACL injury using muscle biopsies of the vastus lateralis muscle that there is an expansion of collagen within the extracellular matrix surrounding muscle fibers (Figure 1)9. However, this technique is invasive and not practical as a screening tool to identify individuals at risk for poor recovery. T1p imaging maybe a possible tool to assess increases in fibrotic tissue within muscle. However, little work has been done in muscle in clinical populations using T1p. We tested the hypothesis that even after ACL reconstruction T1p values remain elevated in the injured leg of patients, and that declining quadriceps muscle strength could be predicted by lengthened T1p times.Methods
6 subjects who had an ACL reconstruction participated in the study (Age 27.5±4.3 years old, weight 72.6±6.9 kg Sex 2M/4F, 4 additional subjects scheduled). All imaging was performed on a 3T MRI scanner (MAGNETOM Trio, Siemens Healthcare, Erlangen, Germany) using a multi element phased array flexible body coil wrapped around the thigh muscles. T1p imaging was acquired with a TR of 5.8 ms, TE 2.5ms, spin lock hold times of (0/10/20/30/40/50/60/70/80/90ms), frequency 300hz matrix of 256x256, slice thickness was10mm thick, 2 averages were taken with 4 shots per slice. Data was then fitted to a mono exponential decay curve using custom code in Matlab ( Natick, MA, USA). The vastus lateralis muscle of the quadriceps muscle was analyzed to be consistent with previous research using muscle biopsy. The subjects’ isometric quadriceps strength was assessed using a Biodex isokinetic dynamometer (Shirley, NY, USA) set to 90 degrees of knee flexion. Strength data was normalized to body weight (kg) and data from both the injured and non-injured legs was examined. Comparisons between the injured and non injured leg were made with an independent t-test and correlations made using Pearson product moment correlations (SPSS Inc, Chicago, IL, USA)Results
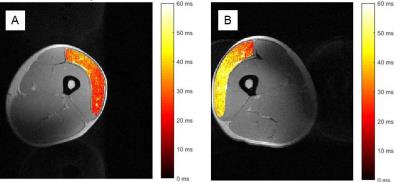
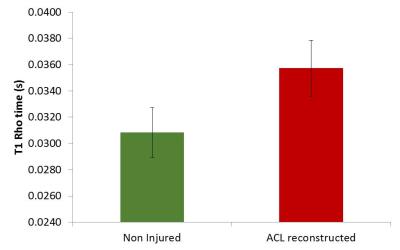
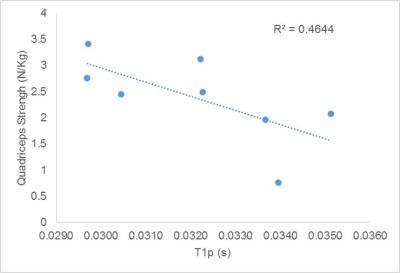
Representative maps of T1p in non-injured and injured legs from one subject are shown in Figure 2 and demonstrate diffuse elevation of T1p times in the injured leg. T1p times were significantly lengthened, on average 15%, in injured legs compared to corresponding internal control legs (Figure 3, p=0.002). Additionally we found a significant correlation between T1p time and quadriceps strength (p=0.03, r=-0.69), with longer times associated with lower strength values (Figure 4). Due to recently having surgery, we were unable to collect quadriceps strength data on 2 subjects.Discussion\Conclusion
The injured leg in subjects with an ACL reconstruction had a significantly longer T1p time. This finding is in agreement with previous work by our laboratory using histochemical techiques of muscle biopsies showing an expansion of collagen within the extracellular matrix around muscle after this injury 9. This report represents a novel application of a T1p imaging sequence in muscle of a clinical population for whom it is difficulty to assess potential causes of continued muscle dysfunction which limits recovery. Additionally, we found that longer T1 rho times were associated with a weaker quadriceps muscle. Thus, the use of T1p could provide important insights regarding the involvement fibrous inclusions as a result of injury which reduces the adaptive capacity and strength of the muscle. Potentially, T1p could be used in helping to guide the planning of surgery and rehabilitation to minimize and address early collagen depositionAcknowledgements
Research reported in the publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health through award number K23AR062069References
1. Griffin, L.Y., et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am. J. Sports Med. 34, 1512-1532 (2006).
2. McLean, S.G. & Beaulieu, M.L. Complex integrative morphological and mechanical contributions to ACL injury risk. Exercise and Sport Science Reviews 38, 192-200 (2010).
3. Mather, I.I.I.R.C., et al. Societal and Economic Impact of Anterior Cruciate Ligament Tears. The Journal of Bone & Joint Surgery 95, 1751-1759 (2013).
4. Lindström, M., Strandberg, S., Wredmark, T., Felländer-Tsai, L. & Henriksson, M. Functional and muscle morphometric effects of ACL reconstruction. A prospective CT study with 1 year follow-up. Scand. J. Med. Sci. Sports, n/a-n/a (2011).
5. Jansson, K.A., Linko, E., Sandelin, J. & Harilainen, A. A prospective randomized study of patellar versus hamstring tendon autografts for anterior cruciate ligament reconstruction. Am. J. Sports Med. 31, 12-18 (2003).
6. Ardern, C.L., Taylor, N.F., Feller, J.A. & Webster, K.E. Return-to-Sport Outcomes at 2 to 7 Years After Anterior Cruciate Ligament Reconstruction Surgery. The American Journal of Sports Medicine 40, 41-48 (2012).
7. Ardern, C.L., Taylor, N.F., Feller, J.A. & Webster, K.E. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. British journal of sports medicine 48, 1543-1552 (2014).
8. Ardern, C.L., Webster, K.E., Taylor, N.F. & Feller, J.A. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. British journal of sports medicine 45, 596-606 (2011).
9. Noehren, B., et al. Cellular and Morphological Alterations in the Vastus Lateralis Muscle as the Result of ACL Injury and Reconstruction. J. Bone Joint Surg. Am. 98, 1541-1547 (2016).
Figures