5126
Quantitative Lower Limb Perfusion Territory Imaging with Vessel Encoded Arterial Spin Labeling1Academy for Advanced Interdisciplinary Studies, Peking University, Beijing, People's Republic of China, 2College of Engineering, Peking University, Beijing, People's Republic of China, 3Department of Radiology, Peking University First Hospital, Beijing, People's Republic of China
Synopsis
Critical limb ischemia (CLI) represents the most severe clinical manifestation of peripheral arterial disease (PAD). It has been proved that l lower extremity arterial stenosis and collateral circulation compensatory ability after occlusion play an important role on CLI. This study proposed a strategy for assessment of lower extremity arterial stenosis and collateral circulation compensatory ability by the noninvasive vessel-encoded arterial spin labeling (VEASL) to quantitatively assess perfusion territory of lower extremity arterial. The lower limb perfusion territory image and the angiosome map were obtained in this study, indicating the potential of VEASL for CLI assessment.
Purpose
Critical limb ischemia (CLI) represents the most severe clinical manifestation of peripheral arterial disease (PAD) and is the major cause of ischemic amputation [1]. It has been proved that lower extremity arterial stenosis and collateral circulation compensatory ability after occlusion play an important role on CLI [2]. This study proposed a strategy for assessment of lower extremity arterial stenosis and collateral circulation compensatory ability by the noninvasive vessel-encoded arterial spin labeling (VE-ASL) to quantitatively assess perfusion territory of lower extremity arterial.Materials & Methods
Subjects and MRI protocol
Two healthy volunteers (one 22-years-old male and one 22-years-old female) were examined with informed consent obtained before each measurement. The study was approved by the local Institutional Review Board and all subjects gave informed consent. All MR images of the prostate cancer were acquired on a clinical 3T scanner (Signa TM; GE Medical Systems, Milwaukee, WI), using a 8 channel knee coil.
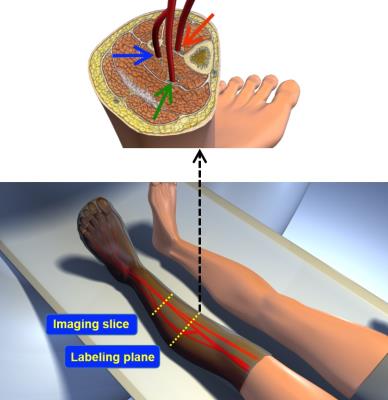
The structure of lower-extremity peripheral arteries (anterior tibial, posterior tibial, and peroneal) was visualized with non-contrast Time-of-Flight MRA sequence: TR/TE = 21/3.2 ms; flip angle = 60°; 1 signal intensity acquired; 98 sections; section thickness = 1.6 mm with a section overlap of 0.8 mm; FOV = 240 mm; matrix size = 384. VEASL: TR/TE = 4000/8.1 ms; labeling duration = 2000 ms; postlabeling delay (PLD) = 1900 ms; section thickness/section gap = 8/2 mm; FOV = 240 mm; matrix = 128. The labeling plane was located 60 mm superior to the imaging slice (Fig.1).
Modified VE-ASL Based on Hadamard Encoding
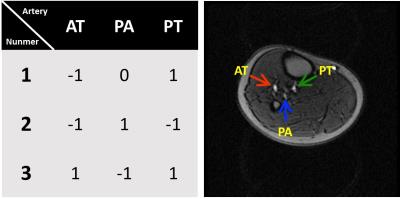
A modified 3-cycle Hadamard encoding schedule was employed to separate three vessels [3]: anterior tibial artery (AT), peroneal artery (PA), and posterior tibial artery (PT) (Fig.2) by utilizing a pseudo-continuous tagging pulse train applied both on transversal and vertical positions. The vessel encoded perfusion images were post-processed by applying Gaussian filter for the reason of low SNR in muscle perfusion imaging.
Statistical Analysis
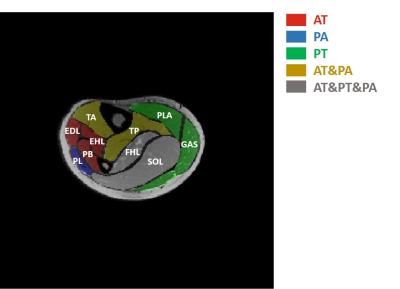
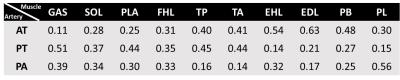
After quantification of territory blood flow, all muscle groups were divided including gastrocnemius (GAS) ; soleus (SOL); plantaris (PLA); flexor hallucis longus (FHL); tibialis posterior (TP); tibialis anterior (TA); extensor hallucis longus (EHL); extensor digitorum longus (EDL); peroneus brevis (PB) and peroneus longus (PL). Percentage of different muscle perfusions from the three vessels were calculated separately and the angiosome map of lower limb was obtained by comparing the weight of the three vessels’ separate perfusion. If the difference of the muscle perfusion percentages between two vessels is above 0.1, the vessel with higher perfusion percentage is taken as the source artery of the muscle.
Results
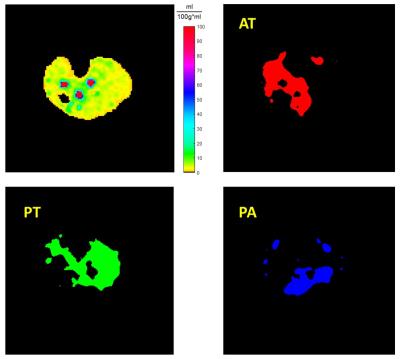
Perfusion maps of the lower limb skeletal muscle with encoded vessels of healthy subjects were obtained. Blood flows territory contributed by vessels AT, PT and PA are colored with red, green and blue respectively in Fig. 3. The average muscle blood flows are 9.15, 9.48 and 13.16 (mL/min/100g) for AT, PT and PA perfusion territory. Also, percentage of different muscle perfusions from the three vessels were calculated separately in Table.1. By comparing the perfusion weight of three vessels, the angiosome source arteries were found and the angiosome map of lower limb was shown in Fig.4.Discussion/Conclusion
The present study evaluated the feasibility of quantitative lower limb perfusion territory imaging with VEASL approach. The angiosome source artery could be found and the angiosome map could be obtained with noninvasive VEASL, which has the potential for CLI assessment. In the future, SNR of ASL imaging needs to be improved for lower limb perfusion imaging.Acknowledgements
No acknowledgement found.References
[1] Davies M G. Methodist DeBakey cardiovascular journal, 2012, 8(4): 10-14.
[2] de Lussanet Q G, et al. NMR in biomedicine, 2006, 19(1): 77-83.
[3] Eric C. Wong. MRM, 2007, 58:1086–1091
Figures