5097
Efficacy of GelrinC in the treatment of chondral and osteochondral lesions: MRI results based on semi-quantitative MOCART scoring and T2 mapping1Department of Orthopaedics, Medical University of Vienna, Vienna, Austria, 2High Field MR Center, Department of Biomedical Imaging and Image-Guided Therapy, Medical University of Vienna, Vienna, Austria, 3Regentis Biomaterials Ltd, Or Akiva, Israel, 4CD Laboratory for Clinical Molecular MR Imaging, Vienna, Austria
Synopsis
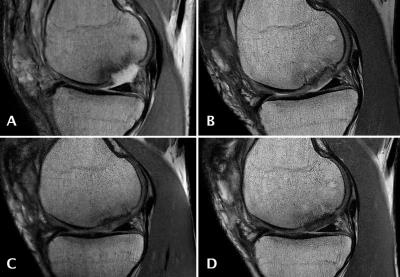
The treatment of femoral cartilage lesions still remains a challenge. Established cartilage repair techniques include microfracture (MFX), acellular scaffolds and cell based therapies such as ACI and MACI, which differ in associated morbidity and outcome. Therefore, there have been strong research efforts to develop novel treatment alternatives. In this study, we demonstrate that GelrinC, a novel acellular biodegradable implant, allows a successful treatment of both chondral and osteochondral femoral lesions in a minimal invasive one-step procedure. For both lesion types a substantial improvement of MOCART scores as well as T2 values has been demonstrated over a 24-month period.
Purpose
Focal cartilage injuries occur frequently and repair remains challenging. Surgical treatment aims to alleviate symptoms, enhance cartilage regeneration and integrity and preclude or delay the onset of osteoarthritis development. Newly available acellular scaffolds have the advantage of requiring only a single surgical procedure and are made from biodegradable synthetic, natural or hybrid polymers. Acellular scaffolds provide a matrix onto which mesenchymal stem cells (MSCs) originating from microfractured subchondral bone and surrounding cartilage, attach, differentiate and develop into new functional tissue.1 The purpose of this study was to evaluate the efficacy of GelrinC, a novel acellular, biodegradable implant, in the treatment of both chondral and osteochondral femoral lesions using semi-quantitative MOCART scoring2 for morphological and T2 mapping for biochemical assessment at 24 months follow up.Subjects and Methods
This study was designed as a single arm, open label, multi-center study conducted in Europe and Israel. MR imaging (1.5/3T) was performed at 1 week (baseline), 6, 12 and 24 months after GelrinC implantation. The morphological imaging protocol consisted of a sagittal proton density (PD) FSE sequence, a coronal PD FSE sequence with fat suppression a 3D gradient echo sequence (not available at all sites) and a sagittal T1-SE sequence. For T2 mapping, a multi-echo-spin echo (CPMG) sequence was used at all sites with 3T MRI scanners. Semi-quantitative MOCART scoring was evaluated for chondral and osteochondral lesions. T2 assessment was based on global T2 (T2 of the repair tissue divided by T2 of healthy reference cartilage) and zonal T2 indexes (T2 of deep cartilage divided by T2 of superficial cartilage).Results
Fifty-six (36 male, 20 female) patients with a mean age of 38 ± 10 years and an average lesion size of 2.42 cm2 ± 1.08 were enrolled in the study. MR imaging at 24 months was available for 42 patients; Of these, 30 patients presented chondral lesions and 12 osteochondral lesions. The average MOCART score for both chondral and osteochondral lesions was 72, 81 and 85 at 6, 12 and 24 months respectively. At 24 months MOCART scores of both chondral (Average MOCART score of 85) and osteochondral (Average MOCART score of 86) lesions were excellent. Due to the restriction to 3T scanners, T2 mapping was available for 32 patients. The global T2 index ranged between 0.8 and 1.2 (normal cartilage) in 7%, 71% and 61% of patients at baseline, 12 and 24 months, respectively. At 24 months chondral and osteochondral lesions showed similar global T2 indices, with1.06 and 1.03 respectively. The zonal T2 index for RT a marker for restoration of the collagen fiber network demonstrated < 20% difference to the zonal T2 index for normal cartilage in: 36%, 62% and 68% patients at baseline, 12 and 24 months, respectively. Chondral and osteochondral lesions showed excellent outcome at 24 month follow up with zonal T2 indices of 1.02 and 1.11 respectively.Discussion and Conclusion
The morphological evaluation of the repaired tissue following GelrinC
implantation showed high MOCART scores throughout the follow up period for the
majority of patients with a significant improvement from the 6 months to the 24
months follow-up (p < 0.001). The biochemical evaluation using T2
mapping demonstrated significant zonal variation, indicative of a reorganization
of the collagen network. When comparing chondral with osteochondral lesions, both
subgroups showed similar MOCART and T2 profiles suggesting that the GelrinC
procedure provides a treatment option for both chondral and osteochondral lesions.Acknowledgements
No acknowledgement found.References
1. E.B. Hunziker, K. Lippuner, M.J. Keel, N. Shintani, An educational review of cartilage repair: precepts & practice--myths & misconceptions--progress & prospects, Osteoarthritis Cartilage 23(3) (2015) 334-50.
2. S. Marlovits, P. Singer, P. Zeller, I. Mandl, J. Haller, S. Trattnig, Magnetic resonance observation of cartilage repair tissue (MOCART) for the evaluation of autologous chondrocyte transplantation: determination of interobserver variability and correlation to clinical outcome after 2 years, Eur J Radiol 57(1) (2006) 16-23.