5096
Predictive value of T2 Mapping for untreated patellar cartilage defects1Department of Orthopaedics, Medical University of Vienna, Vienna, Austria, 2High Field MR Center, Department of Biomedical Imaging and Image-Guided Therapy, Medical University of Vienna, Vienna, Austria, 3Department of Biomedical Imaging and Image-Guided Therapy, Medical University of Vienna, Vienna, Austria, 4CD Laboratory for Clinical Molecular MR Imaging, Medical University of Vienna, Vienna, Austria
Synopsis
Assessment and adequate treatment of articular cartilage lesions are a common challenge in clinical orthopaedic routine. To allow for better disease prediction and thus evidence-based treatment selection, there is a strong need for objective predictive markers. In this study we demonstrate the predictive potential of T2 mapping in the assessment of untreated patellar cartilage lesions over an average follow up time of four years.
Purpose
Articular
cartilage lesions remain a challenge in orthopaedic practice. To improve
treatment decision and to allow for a more exact prognosis, there is strong
demand for predictive imaging biomarkers. It has been shown that even before morphological changes become evident, biochemical changes of the extracellular matrix might occur.1 T2 mapping is sensitive to water content and collagen ultrastructure of articular cartilage2 and thus bears the potential to assess these changes. The purpose of this study was to
assess the predictive value of T2 mapping in patients with untreated focal
patellar cartilage lesions regarding defect progression in a mean follow-up of
four years.
Subjects and Methods
This study
was approved by the local ethics committee and written informed consent was
obtained from all patients prior to enrolment. We aimed to recruit thirty
patients, who previously underwent an MRI examination for anterior knee pain or
suspected patellar cartilage defects at our institution. This baseline MRI
examination had to include T2 mapping (CPMG) (resolution = 0.4x0.4x3.0 mm;
TR=1200; eight echo times (TE) in the range from 13.8 to 82.8 ms, measurement
time 4:09 min) and an axial proton density weighted turbo-spin-echo sequence
(resolution = 0.2x0.2x2.0 mm; TR/TE=2400/36 ms, measurement
time: 6:11 min). Furthermore, only patients who did not receive any surgical
treatment of the respective knee joint in the meantime were included in order
to avoid any bias due to surgical intervention. At follow up, patients were
examined again using the exact same protocol on the same scanner with the same
knee coil. In each patient, the most severe patellar cartilage lesion was
graded on the axial PD TSE images of the baseline as well as the follow-up
examination according to the ICRS grading system. Furthermore, T2 maps were
evaluated based on a region-of-interest (ROI) analysis. To do so, the
respective defect extents were defined on the morphological PD TSE images of
the follow-up examination. The ROIs were subsequently transferred to the T2
mapping follow-up and baseline exams. In addition, a healthy reference
cartilage region was defined and evaluated in each patient in the baseline and follow-up
exams as internal reference. Differences in the T2 values according to ICRS
grading were evaluated using one-way ANOVA with post hoc Tukey test. The
predictive values of the global T2 values at baseline regarding future defect
progression in the interval was assessed with a ROC analysis. All statistical
evaluations were performed using IBM SPSS 23.0. A p-values smaller 0.05 was
considered to be statistically significant.
Results
Thirty
patients (mean age, 36.7 ± 11.1 years; 16 males, 14 females) were
included in the study. The average follow-up time between the baseline and follow-up
examination was 4.0 ± 1.6 years. At baseline, ten patients had no
defect, 12 patients had a grade 1 defect and 8 patients had a grade 2 defect based
on morphological images. Global T2 values correlated well with the defect
grades with an average T2 of 40.3 ms for grade 0, 48.5 ms for grade 1
defects and 55.6 ms for grade 2 defects (p < 0.01). Regarding
the morphological ICRS grading, 17 patients remained constant over the follow
up period whereas 11 patients showed a defect progression of one or more ICRS
grades. Patients who showed defect progression in the interval had
significantly higher global T2 values at baseline (57.5 ms) than patients
who did not show defect progression (40.6 ms) (p < 0.01).
Furthermore, patients who remained constant over the follow-up time regarding
the ICRS grading, showed only a minor increase in T2 relaxation times from 40.7 ms
at baseline to 43.1 ms at follow-up.
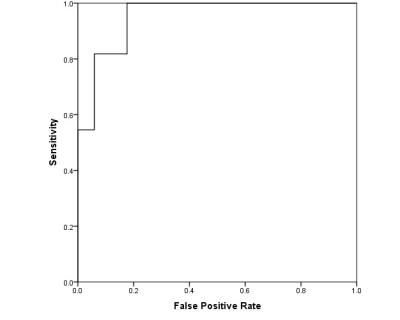
The ROC
analysis (Figure 2) showed an area under the curve of 0.95, demonstrating that
global T2 value may serve as a good predictor for defect progression in
low-grade cartilage defects.Discussion
This study provides evidence regarding the possible potential of T2 mapping as a predictive marker for patellar cartilage degeneration in untreated defects. Furthermore, it confirms previous observations3 that T2 relaxation times correlate well with the ICRS grade of cartilage degeneration. Moreover, it demonstrates that T2 relaxation times in patellar cartilage remain relatively constant over time in patients with stable cartilage conditions.Acknowledgements
No acknowledgement found.References
1.Choi JA et al., MR Imaging of articular cartilage physiology. Magn. Reson Imaging Clin N Am 2011;19:249-28
2. Mosher T.J. et al., Cartilage MRI T2 relaxation
time mapping: overview and applications, Semin Musculoskelet Radiol 8(4) (2004)
355-68.
3. Apprich S et al., Quantitative T2 mapping of the patella at 3.0T is sensitive to early cartilage degeneration, but also to loading of the knee, Eur J Radiol 81(4) (2012) e438-43.