5021
Feasibility of synthetic MRI in knee in routine practice: image quality and diagnostic accuracy1Geneva University Hospitals, Geneva, Switzerland
Synopsis
Synthetic MRI is a very promising method to generate different contrasts used in clinical practice from quantitative T1, T2 and PD measurements. In this study we confirmed the feasibility of Synthetic MR in knee examinations, allowing generation of T1, PD and STIR images in faster time than conventional imaging with appropriate quality and good diagnosis confidence.
Introduction
Synthetic MR is a method allowing reduction of examination time and access to quantitative imaging. It has already been validated in cerebral applications1, notably in multiple sclerosis2. In musculoskeletal field, this technique is promising in standard protocols like knee. The aim of this study is to assess the image quality and the diagnostic accuracy compared to conventional MRI in patients with post traumatic or degenerative knees.Material and methods
Twenty patients underwent knee MRI to exclude
meniscal, ligamentous or cartilaginous injuries. Syntac sequence was added to the
standard protocol (coronal T1 and Short TI Inversion Recovery (STIR), sagittal proton
density (PD)) in Philips 1.5 MR scanner. The
syntac sequence is based on a TSE sequence with a saturation pulse (120°) and 4
different inversion times and 2 echo times which lead to 8 images with
different contrasts. These images are used by SyMRI v8 software (SyntheticMR AB, Linköping, Sweden) to generate quantitative T1, T2 and PD images and
then create synthetically T1, PD and STIR weighted images with user chosen
TE/TR/TI. Sequence
parameters were : sagittal orientation, FOV 200x150 mm, acquisition
(reconstruction) voxel size 0.45x0.59 (0.45x0.45) mm, 20 slices of 5mm
with no gap, TE 13 / 100 ms, TR 3106 ms, TSE factor 10, SENSE acceleration
factor 1.5. The acquisition time of the synthetic sequence was 7min8sec. In
this study we choose TE/TR to match the conventionnal sequences and TI adequate
to suppress the fat signal in the image. Blinded MSK radiologist evaluated by using 3 points
score the overall sequence quality (poor, fair, good), the visualisation
of anatomic structures (bone, cartilage, meniscus, cruciate ligaments anterior
and posterior and extensor tendons) and the presence of artefacts. In addition
final diagnosis was compared to conventional MRI.Results
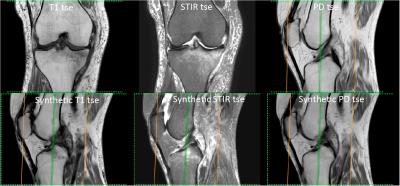
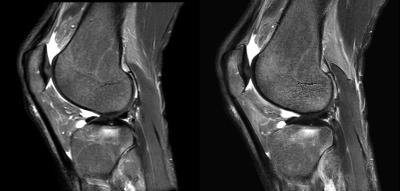
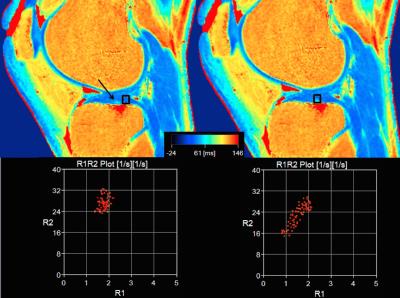
The syntac sequence was acquired in 39% less time than the conventional MR imaging. Sagittal Synthetic PD-, T1- and STIR-weighted images were rated as fair (5%, 20%, 5% respectively) or good quality (95%, 80%, 95%) despite the presence of popliteal artery pulsations artifacts in all cases, severe in 50% of cases. Cartilage, meniscus and tendons were well visualised in all cases in Synthetic T1, PD and STIR (figure 1). Qualitative assessment of bone oedema was rated as good in Synthetic STIR as illustrated by figure 2. Cruciate ligaments visualisation was rated as poor in 15%, 30% and 60% of cases on DP, STIR and T1 sequences respectively because of the inadequate visualisation of the anterior cruciate ligament, despite the good visualisation of the posterior cruciate ligament in all cases. This was attributed to the slice thickness (5 mm in Synthetic MR, 3mm in conventional PD sag) without impact on radiological diagnosis. Finally, diagnostic accuracy was identical than in conventional MR in all cases. In this study, T1 and T2 mapping were available but not directly evaluated, however as an example in a patient with a cartilage lesion, R1 (1/T1) versus R2 (1/T2) plot show the dispersion of values in the lesion compared to a normal surrounding area (figure 3).Discussion
In this preliminary study, synthetic MR images alone gave satisfying diagnostic confidence, with a globally good image quality. The main limitations are vascular flow artifacts as well as slice thickness for the interpretation of smaller structures. Also, it is evident that a single sequence may not be sufficient to explore the structures of the whole knee, so an additional plane may be acquired either with a conventional sequence or with the synthetic method. In this study, the potential use of quantitative T1 and T2 values was not fully explored. T2 mapping is already of great interest for cartilage assessment and can thus be obtained without additional acquisition time. Moreover, combination of quantitative T1 and T2 is also bringing new information that are completely independent of the MR technique and that are expected to be more accurate and relevant than traditional MRI following a recent publication from the European Society of Radiology3. This will be explored in the next steps of the study.Conclusion
Our pilot study confirmed the feasibility of Synthetic MR in knee examinations, allowing generation of T1, PD and STIR images in faster time with appropriate quality and good diagnosis confidence. This is an important step toward clinical integration of quantitative MRI in standard protocols.Acknowledgements
No acknowledgement found.References
1. Blystad I, Warntjes JB, Smedby O, et al. Synthetic MRI of the brain in a clinical setting. Acta Radiol. 2012 Dec 1;53(10):1158-63.
2. Granberg, T, Uppman, M, Hashim, F, et al. Clinical Feasibility of Synthetic MRI in Multiple Sclerosis: A Diagnostic and Volumetric Validation Study. American Journal of Neuroradiology, 2016 ; 1–7.
3. European Society of Radiology (ESR). Magnetic Resonance Fingerprinting - a promising new approach to obtain standardized imaging biomarkers from MRI. Insights into Imaging, 2015, 6(2), 163–165.
Figures