5019
3D IR-UTE-Cones for High Contrast MR Imaging of Lamellar Bone1Department of Radiology, University of California, San Diego Medical Center, La Jolla, CA, United States, 2Orthopedic Surgery, Scripps Clinic, La Jolla, CA, United States, 3Radiology Service, VA San Diego Healthcare System, San Diego, CA, United States
Synopsis
Lamellar bone is poorly evaluated using conventional magnetic resonance (MR) imaging secondary to its inherently short T2 relaxation time. Rather, the contours of lamellar bone are often inferred based on marrow signal. In the setting of shoulder instability or pre-operative planning for arthroplasty, rotator cuff integrity and glenoid bone defects are frequently assessed using both MRI and computed tomography (CT), respectively. An MR imaging technique to directly image lamellar bone could potentially eliminate the need for a CT scan and be particularly useful for young patients with acute shoulder instability.
Purpose
To optimize the 3D Inversion Recovery prepared Ultrashort-Echo-Time with Cones Readout (IR-UTE-Cones) technique for direct imaging of lamellar bone using CT as a gold standard.Methods
Three cadaveric shoulder specimens (mean age 83 years), two healthy volunteers (mean age 28 years) and one patient planned for shoulder arthroplasty (age 63) were imaged on a clinical 3T scanner (Signa HDx, GE Healthcare, Milwaukee, WI) using a shoulder coil and a conventional clinical imaging protocol. In addition, the 3D IR-UTE-Cones sequence, which utilizes an adiabatic inversion recovery pulse followed by UTE acquisition (TR 110-134 ms, TE 0.03 µs, FA 26, and FOV 20 cm). Inversion time (TI), matrix, number of projections, number of signal averages, and acquisition imaging plane were varied to determine the effect on image quality. CT was subsequently performed using a 64-slice scanner (VCT, GE Healthcare, Milwaukee, WI). Registration of the CT and 3D IR-UTE-Cones MR images was performed after binary thresholding and linear registration via the FSL FLIRT program (FMRIB’s Linear Registration Tool). Source and registered images were qualitatively evaluated and compared by a musculoskeletal radiologist.Results
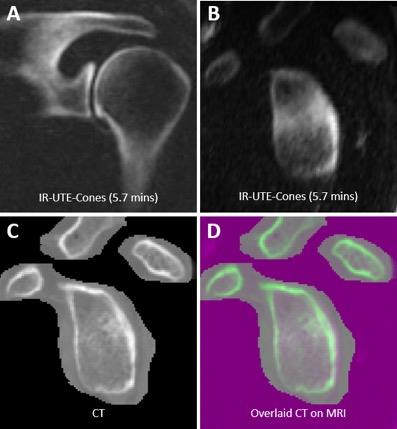
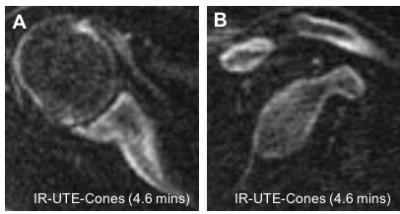
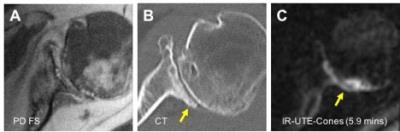
On conventional MR images, lamellar bone showed no discernable signal. However, the 3D IR-UTE-Cones sequence demonstrated high-contrast imaging of lamellar bone. Maximal suppression of both fat and water (including muscle and edema) was achieved using TR/TI of 134/54-58 ms for cadaveric specimens (Figures 1 and 2) and 110/46 ms for in vivo imaging (Figures 3 and 4). CT-MR dataset registration confirmed that there was near-perfect registration between the two modalities when using 3D IR-UTE-Cones (Figure 2D). High-quality images could be generated using the 3D IR-UTE-Cones sequence with resolution and imaging time approaching conventional 2D MR sequences. However, isotropic voxel size could not be accomplished in clinically compatible imaging times.Discussion
Imaging plays a major role in the preoperative assessment of patients with shoulder instability or osteoarthritis. In particular, when evaluating for the presence and severity of osseous injuries, several studies have showed that both CT and MR can accurately quantify bone loss.1,2 While 3D CT of the shoulder has been the imaging gold standard for the depiction of complex glenoid anatomy, MR is the first-line imaging modality for the identification of soft tissue lesions involving cartilage, capsulolabral complex, and rotator cuff.3-5 We therefore sought to optimize the 3D IR-UTE-Cones sequence for the depiction of lamellar bone in the shoulder and potentially minimize the need for preoperative CT.
Cortical bone consists of three pools of protons, including pore and collagen-bound water as well as collagen methylene protons.6 In distinction to conventional MRI, UTE sequences are capable of detecting signal from both pore and collagen-bound water (T2* values from collagen methylene protons are extremely short and this pool remains “invisible”). The 3D Cones sequence provides volumetric UTE imaging with improved signal-to-noise ratio efficiency compared to 2D or 3D radial UTE sequences as well as significantly reduced scan times due to anisotropic field of view and spatial resolution. This sequence follows an adiabatic inversion pulse, which provides relatively uniform inversion given its relative insensitivity to B1 inhomogeneities. When combined with an appropriate TR and TI, this inversion pulse has been shown to reduce fat and muscle signal by greater than 80%, while short T2 magnetization is only partially saturated.7 Therefore, direct imaging of lamellar bone can be achieved through efficient suppression of long T2 fat and water components.
We present a novel application of this technique in the shoulder, where glenoid bone contours acquired using the 3D IR-UTE-Cones technique corresponded nearly perfectly to CT and were complimentary to conventional MRI. However, if high-resolution isotropic voxel size is necessary, such as for 3D surface rendering of lamellar bone, CT should be performed.
Conclusion
Direct and selective imaging of lamellar bone in the shoulder can be performed using the 3D IR-UTE-Cones technique in clinically feasible imaging times.Acknowledgements
The authors acknowledge grant funding from the VA Clinical Science R&D Service (Merit Award I01CX001388) and the NIH (1R01AR068987).References
1. Gyftopoulos S, Beltran LS, Yemin A, Strauss E, Meislin R, Jazrawi L, et al. Use of 3D MR reconstructions in the evaluation of glenoid bone loss: a clinical study. Skeletal Radiol. 2014;43(2):213-8.
2. Rerko MA, Pan X, Donaldson C, Jones GL, Bishop JY. Comparison of various imaging techniques to quantify glenoid bone loss in shoulder instability. J Shoulder Elbow Surg. 2013;22(4):528-34.
3. Gusmer PB, Potter HG, Schatz JA, Wickiewicz TL, Altchek DW, O'Brien SJ, et al. Labral injuries: accuracy of detection with unenhanced MR imaging of the shoulder. Radiology. 1996;200(2):519-24.
4. Hayes ML, Collins MS, Morgan JA, Wenger DE, Dahm DL. Efficacy of diagnostic magnetic resonance imaging for articular cartilage lesions of the glenohumeral joint in patients with instability. Skeletal Radiol. 2010;39(12):1199-204.
5. Jana M, Gamanagatti S. Magnetic resonance imaging in glenohumeral instability. World J Radiol. 2011;3(9):224-32.
6. Chang EY, Bae WC, Shao H, Biswas R, Li S, Chen J, et al. Ultrashort echo time magnetization transfer (UTE-MT) imaging of cortical bone. NMR Biomed. 2015;28(7):873-80.
7. Du J, Bydder GM. Qualitative and quantitative ultrashort-TE MRI of cortical bone. NMR Biomed. 2013;26(5):489-506.
Figures