5002
Study of correlation between multifidus muscles atrophy and degenerative diseases of lumbar spine in patients with low back pain using MRI1Affiliated hospital of Qingdao University, Qingdao, People's Republic of China, 2Department of Radiology, stony brook university hospital, Stony brook, NY, United States
Synopsis
Multifidus muscles (MF) atrophy are common in patients with Low back pain (LBP). Degenerative diseases of the lumbar spine, such as disc herniation, disc degeneration and facet joint osteoarthritis, are leading cause of LBP. Various studies have previously focused on the relationship between MF atrophy and disc degeneration, disc herniation. However, the results are inconsistent. Besides, no study for the correlation between MF atrophy and facet joint osteoarthritis has previously been conducted. This study will investigate the correlation between MF atrophy and disc degeneration, disc herniation, facet joint osteoarthritis using MRI.
PURPOSE
There is a known, but not thoroughly evaluated association between fatty degeneration of para-spinal muscle and low back pain (LBP).1-9 Most prior studies have focused on the multifidus muscle (MF), because of its contribution to lumbar spine segmental stability.10 Additionally, most of the previously studied populations involves patients with radiculopathy, 1, 3-4, 11 disc herniation5, 12 Moreover, these prior results are inconsistent. Hence the aim of this study is to investigate potential correlation between MF atrophy and MR signs of lumbar spine degeneration in patients with LBP.METHODS
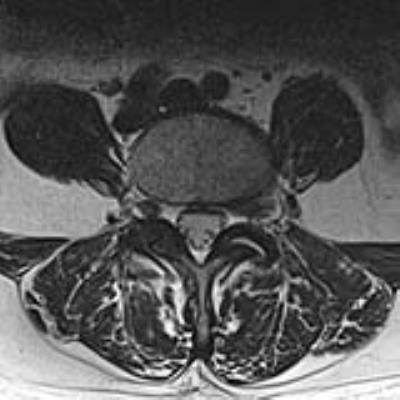
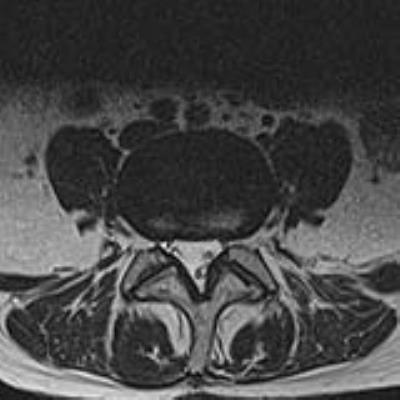
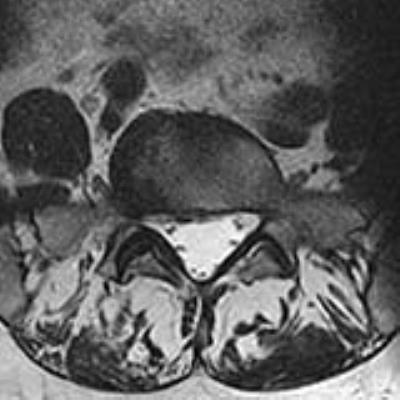
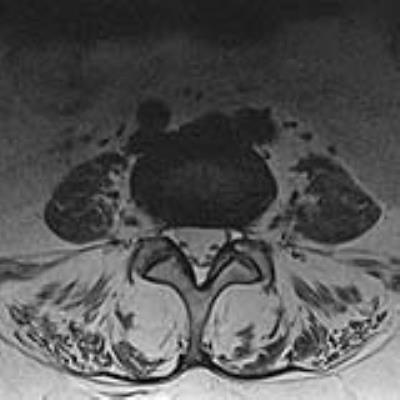
Following IRB approval, patients who had low back pain and an MRI of lumbar spine between June 2015 and July 2016, were evaluated. Patients with deformity (scoliosis, spondylolisthesis, kyphosis, pars defects) or history of lumbar spine surgery were excluded. 518 patients (278 females and 240 males; age, 10-92 years; mean, 49.99±17.596 years) were identified and their MRI studies were retrospectively reviewed by a radiologist twice with a one-month washout period. MF atrophy was graded at L4-5 and L5-S1 levels (largest diameter at these levels, allowing for a better evaluation) according to the Goutallier classification (Fig. 1-4). Disc degeneration was graded according to Pfirrmann classification, and facet joint osteoarthritis was graded according to Fujiwara classification. Disc herniation was assessed by NASS criteria. These patients were further classified into two groups according to clinical presentations. One group was simple low back pain, the other group with superimposed radiculopathy. Age, gender, height, and weight were also recorded. Significance level was set at P<0.05. Multinomial logistic regression was used to evaluate relationship between fatty degeneration of MF and radiculopathy, age, gender, height, weight, signs of lumbar spine degeneration. Spearman correlation coefficient was calculated. Intra-observer agreement was tested as well.RESULTS
At both L4-5 and L5-S1 levels, significant correlation is demonstrated between MF atrophy with age, gender, and facet joint osteoarthritis, at L4-L5 level, P<0.001 with correlation coefficients of 0.652, 0.244, and 0.509 respectively. At L5-S1 level, there were similar correlations between MF atrophy with age (P<0.001), gender (P<0.001), facet joint osteoarthritis (P=0.002), with correlation coefficients were 0.546, 0.368, and 0.354 respectively. Additionally, at the L5-S1 level, there was a significant correlation between MF atrophy and disc degeneration (P=0.034) with a correlation coefficient at 0.348. No correlation was found between MF atrophy with height, weight, and disc herniation at both L4-L5 and L5-S1 levels. (At the L4-5 level (p =0.072, 0.233 and 0.603 respectively with at the L5-S1 level p = 0.096, 0.762, and 0.565 respectively)). At L4-L5, there was also no correlation between MF atrophy and disc degeneration (P= 0.198). There is no correlation between MF atrophy and radiculopathy at both level s of L4-L5 and L5-S1 levels with P values at 0.305 and 0.663 respectively. For intra-observer agreement, classification of MF atrophy (Kappa value=0.626, 0.617), disc degeneration (Kappa value=0.556, 0.553), disc herniation (Kappa value=0.619, 0.485), and facet joint osteoarthritis (Kappa value=0.598, 0.677) at L4-5, L5-S1 levels respectively.DISCUSSION
We have demonstrated that increasing age and female gender are both associated with MF atrophy at both L4-L5 and L5-S1 levels. However, there is no correlation between heights, weight with MF atrophy. In term of disc degeneration, correlation with MF atrophy was only found at L5-S1 but not at the L4-5 level. Though, facet osteoarthritis was found to have significant correlation with MF atrophy at both L4-L5 and L5-S1 levels, surprisingly no correlation was found between disc herniation and radiculopathy with fatty replacement of MF. Spine pain is related to the pattern of spinal innervation. Ventral spinal elements (disc/annulus) are innervated separately from posterior spinal elements (facet joints, posterior muscles). 13, 14 The facet joints and MF are supplied by median branch of dorsal ramus which supplies the posterior innervation. This pattern of spinal innervation may explain the correlation between MF atrophy and facet joint osteoarthritis as well as the lack of correlation between radiculopathy and disc degeneration with MF atrophy.CONCLUSION
The relationship between MF atrophy and degenerative diseases of lumbar spine is complicated. However, our large study indicates that MF atrophy positively correlates with advanced age, female gender and facet osteoarthritis, in the lower lumbar spine, but not with disc herniation in patients with local back pain. This data has potential at guiding clinical treatment in certain disease population. Therefore, further study will be required to elucidate the role of MF atrophy in degenerative process of lumbar spine.Acknowledgements
The authors thank Kenneth, Wengler Thomas (Biomedical Engineering,Stony Brook university hospital) for his technical support, Xiaona Xia (Department of radiology,Qilu hospital of Shandong university,Qingdao) for statistical advice, and Wenjian Xu (Department of radiology,Affiliated hospital of Qingdao University) for his writing advice.References
1. Barker KL, Shamley DR, Jackson D. Changes in the cross-sectional area of multifidus and psoas in patients with unilateral back pain: the relationship to pain and disability. Spine. 2004;29(22):515-519.
2. Danneels LA, Vanderstraeten GG, Cambier DC, Witvrouw EE, De Cuyper HJ. CT imaging of trunk muscles in chronic low back pain patients and healthy control subjects. European spine journal. 2000; 9(4):266-272.
3. Hides J, Gilmore C, Stanton W, Bohlscheid E. Multifidus size and symmetry among chronic LBP and healthy asymptomatic subjects. Manual therapy. 2008; 13(1):43-49.
4. Hides JA, Stokes MJ, Saide M, Jull GA, Cooper DH. Evidence of lumbar multifidus muscle wasting ipsilateral to symptoms in patients with acute/subacute low back pain. Spine. 1994;19(2):165-172.
5. Hyun JK, Lee JY, Lee SJ, Jeon JY. Asymmetric atrophy of multifidus muscle in patients with unilateral lumbosacral radiculopathy. Spine. 2007; 32(21):598-602.
6. Kader DF, Wardlaw D, Smith FW. Correlation between the MRI changes in the lumbar multifidus muscles and leg pain. Clinical radiology. 2000;55(2):145-149.
7. Mengiardi B, Schmid MR, Boos N, et al. Fat content of lumbar paraspinal muscles in patients with chronic low back pain and in asymptomatic volunteers: quantification with MR spectroscopy. Radiology. 2006;240(3):786-792.
8. Parkkola R, Rytokoski U, Kormano M. Magnetic resonance imaging of the discs and trunk muscles in patients with chronic low back pain and healthy control subjects. Spine. 1993;18(7):830-836.
9. Ploumis A, Michailidis N, Christodoulou P, Kalaitzoglou I, Gouvas G, Beris A. Ipsilateral atrophy of paraspinal and psoas muscle in unilateral back pain patients with monosegmental degenerative disc disease. The British journal of radiology. 2011;84(1004):709-713.
10. Freeman MD, Woodham MA, Woodham AW. The role of the lumbar multifidus in chronic low back pain: a review. PM & R: the journal of injury, function, and rehabilitation. 2010;2(2):142-146.
11. Campbell WW, Vasconcelos O, Laine FJ. Focal atrophy of the multifidus muscle in lumbosacral radiculopathy. Muscle & nerve. 1998;21(10):1350-1353.
12. Kulig K, Scheid AR, Beauregard R, Popovich JM, Jr., Beneck GJ, Colletti PM. Multifidus morphology in persons scheduled for single-level lumbar microdiscectomy: qualitative and quantitative assessment with anatomical correlates. American journal of physical medicine & rehabilitation. 2009;88(5):355-361.
13. Groen GJ, Baljet B, Drukker J. The innervation of the spinal dura mater: anatomy and clinical implications. Acta neurochirurgica. 1988;92(1-4):39-46.
14. Groen GJ, Baljet B, Drukker J. Nerves and nerve plexuses of the human vertebral column. The American journal of anatomy. 1990;188(3):282-296.
Figures