4997
Paraspinal Muscle Changes with Chronic Low Back Pain by Using 3.0T MR Diffusion Tensor Imaging Technology1Radiology, Peking University Third Hospital, Beijing, People's Republic of China, 2GE Healthcare, MR Research China, Beijing, People's Republic of China
Synopsis
The purpose of the current study is to assess the potential difference of multifidus muscle between non-specific chronic low back pain patients and the healthy individuals using DTI and to compare the sensitivity of DTI to conventional lumbar MRI in detecting muscle pathological changes. DTI and conventional MRI parameters were obtained including FA, ADC, MD and tCSA, fCSA, fCSA/tCSA ratio. Compared to the healthy individuals, NCLBP patients demonstrated differences in DTI parameters of bilateral multifidus muscles. We conclude that DTI is more sensitive in detecting paraspinal muscle pathological changes in the early stage of lumbar degeneration than conventional lumbar MRI.
Purpose
The purpose of the current study is to assess the potential difference of multifidus muscle between non-specific chronic low back pain patients and the healthy individuals using DTI and to compare the sensitivity of DTI to conventional lumbar MRI in detecting muscle pathological changes.Introduction
Paraspinal muscles play an important role in the progression of degenerative chronic low back pain (CLBP). Using conventional lumbar MRI, CLBP patients have demonstrated reduced paraspinal muscle volume and muscle fatty tissue infiltration. However, the morphological change of lumbar spine and paraspinal muscle is limited at the early stage of lumbar degeneration, which prevents conventional MRI from differentiating between the healthy individuals and CLBP patients. Diffusion tensor imaging (DTI) is an emerging MRI technique for evaluating the microstructures and functions of well-organized biologic tissues such as skeletal muscles.Material and Methods
Ten male participants (21-24 year-old, BMI 20.79±1.87) were recruited in the current study. Five participants had non-specific chronic low back pain (NCLBP group) in the past year, with at least 3 months of pain duration in each episode. The other five were asymptomatic (control group) in 3 years preceding the study. All the participants had average daily physical activity and were prevented from performing strenuous exercise in the 24 hours prior to MR examination. All the subjects were instructed to lie in a supine position on the MR examination table for 30minutes before scanning. MRI scans were performed using a 3.0T MRI scanner (MR750w, GE Healthcare), including conventional T1WI, T2WI lumber MRI and axial DTI scans of the L4-S1 vertebrae.
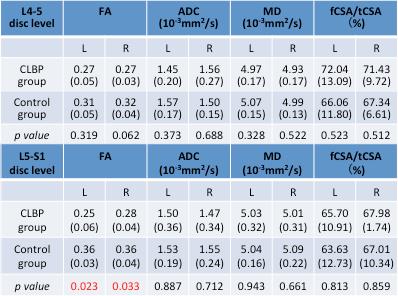
DTI scanning was achieved with a b-value of 400s/mm2 in 15 optimized diffusion encoding gradient directions1. Tensor analyses were performed for background suppression and correction for eddy current distortions using Functool on the GE AW workstation. Regions of interest (ROI) were manually drawn to trace the margins of the bilateral multifidus muscles on post-processed DTI b=0 images at the level of L4-S1 disc level. The mean values of FA, MD and ADC within the ROI were extracted and displayed on the corresponding colored-maps (Figure.1).
Muscle morphological measurements were obtained from the T2WI axial images using ImageJ, including total muscle cross-sectional area (tCSA), functional cross-sectional area (fCSA) and fCSA/tCSA ratio (fCSA/tCSA) at the same disc level with DTI (Figure.2). Statistical analyses were performed using SPSS21.0. Inter-group comparisons were tested using independent-samples t test. P < 0.05 was considered statistically significant.
Results
There was no observed difference in gender, age or BMI between NCLBP and the control groups. None of the subjects demonstrated any sign of lumbar degenerative diseases or abnormal intensity in paraspinal muscle on conventional MRI. At L4-S1 disc level, the average fCSA/tCSA ratio of bilateral multifidus muscles in NCLBP group were larger than that of control group, but with no statistical significance. FA, ADC and MD of the bilateral multifidus in NCLBP group were all smaller than that of the control group at L4-S1 disc level, respectively. There was a significant difference (P=0.016) in average FA of bilateral multifidus at L5-S1 disc level between NCLBP (0.26±0.04) and the control group (0.36±0.03) (Table.1).Discussion
The current study showed that the multifidus FA value of NCLBP patients was significantly lower than that of the control group in L5-S1 disc level. FA reflects the degree of anisotropy in the tissues. According to the stability theory of the spine, paraspinal muscle compensates to the lumbar function restriction due to chronic low back pain and hence leads to muscle strain2. The swollen muscle fiber possesses lower anisotropy, which may explain the observed decreased FA value in the NCLBP group3. The MD value of NCLBP group was in the trend of decrease overall, but below statistical significance. MD indicates the directional average of the diffusion on three main orthogonal directions inside the tissues. In the swollen myocytes, there is a significant decrease in diffusivity on the radial direction (main diffusion direction) and a slightly increase on axial direction, resulting in a reduced MD while averaging the values of all directions4.
Moreover, we demonstrated that the conventional MRI had a limited sensitivity of muscle lesion detection. The fat-saturated T2-weighted images are only capable to detect the discrepancies caused by hyper-intensity of the muscle after the muscle strain deteriorates and further converts into a large amount of interstitial fluid.
Conclusion
In conclusion, NCLBP patients demonstrated differences in DTI parameters of bilateral multifidus muscles compared to the healthy individuals. DTI is more sensitive in detecting paraspinal muscle pathological changes in the early stage of lumbar degeneration than conventional lumbar MRI.Acknowledgements
No acknowledgement found.References
[1] Gravin JEG, Dinesh KA. Quantitative DTI Assessment in Human Lumbar Stabilization Muscles at 3 T. J Comput Assist Tomogr, 2013, 37(1): 98-104.
[2] Panjabi MM. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. Journal of spinal disorders, 1992, 5(4): 383-389; discussion 397.
[3] Budzik J, Balbi V, Verclytte S, et al. Diffusion Tensor Imaging in Musculoskeletal Disorders. Radiographics, 2014, 34(3): E56-72.
[4] Oudeman J, Nederveen AJ, Strijkers GJ, et al. Techniques and applications of skeletal muscle diffusion tensor imaging: A review. J Magn Reson Imaging, 2016, 43(4): 773-788.
Figures