4982
Dynamic MRI For Bowel Motility Imaging – How Fast And How Long?1Department of Radiology, Academic Medical Center (AMC), Amsterdam, Netherlands, 2Centre for Medical Imaging, University College London (UCL), London, United Kingdom
Synopsis
Dynamic (cine) MRI of bowel motility is now routinely performed in clinical practice and advances in post-processing have enabled robust quantitation of this data facilitating numerous research applications. Generally, motility sequences are acquired in a 20 second breath hold at a temporal resolution of 1 fps. In this study, we investigate these core assumptions and provide guidance information for future studies. In summary, we show that a temporal resolution of at least 1 fps is necessary for a scan duration of at least 10 seconds. This is consistent with the majority of small bowel motility studies to date.
Purpose
Intestinal motility, is an essential physiological process that moves
food through the gut but frequently becomes deranged in disease. Hypo-motile segmental
contractility in Crohn’s disease is a powerful biomarker of inflammation, whereas
global pan-enteric changes are seen in neurological conditions including
Parkinson’s disease and Chronic Intestinal Pseudo-Obstruction and changes in
the coordination of contractile activity likely underpin common conditions such
as constipation.1-3 There has been a rapid expansion in the
exploration of dysmotility with MRI due to its availability and cost
effectiveness. Furthermore, improvements in post-processing technologies now
enable fast quantification, providing new insights into gut motility and its
impact in health and disease.4-8
Despite the expansion in the use of MRI, key assumptions regarding 1)
temporal resolution and 2) duration of
the sequence data acquisition widely used in this research have yet to be
rigorously tested. For example, is 1 image per second fast enough to capture a
contractile action? Is a breath-hold of 20 seconds long enough to produce a
consistent motility score? In this study, we implement an accelerated 10 image
per second sequence to ‘over-sample’ bowel motility and quantify these data
using a registration based technique to provide guidance information on
temporal resolution and scan duration in small bowel motility assessment.Methods
Subjects: Six healthy volunteers, 3 male, median age 22 [21-25] were recruited. Scan preparations: All volunteers fasted for 7 hours and ingested 1L of 2.5% mannitol solution over 30 min. prior to the MRI scan. The mannitol was ingested at regular intervals of 10 min., the last of the solution was consumed before entering the scanner room.
Scanner setup: 3T Philips Ingenia MRI scanner. A coronal 2D balanced FFE sequence was used during a breath hold in supine position, using the following sequence parameters: TR/TE=1.9/0.98ms, flip-angle=20o, FOV=400x400mm and spatial resolution of 2.5x2.5x10mm and a temporal resolution of 10 fps.
Image registration: The dynamic series was registered with an optic flow based technique called GIQuantTM (Motilent, Ford, UK) for bowel motility assessment. The motility metric used assessed the standard deviation of the deformation fields’ Jacobian determinant averaged across a region of interest4 henceforth referred to as the mean motility index score (MIS).
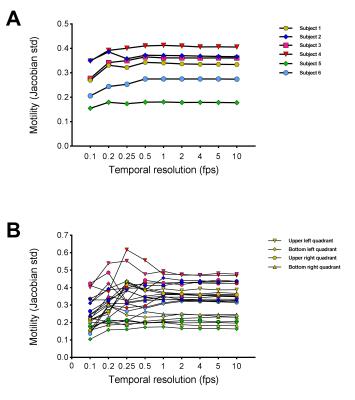
Experiment 1: Temporal resolution - the MRI measurement was retrospectively adjusted by discarding images at regular points in the dataset to create the following temporal resolutions: 10, 5, 4, 2, 1, 0.5, 0.25, 0.2, 0.1 fps (1 image every 10 seconds). The mean MIS values, based on ROI placements described below, were calculated for each temporal resolution.
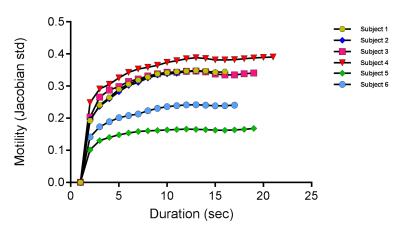
Experiment 2: Scan duration – The dynamic series were re-sampled to 1 image per second and registered. The motility score was calculated from durations of data ranging from 2 seconds up to 20 seconds (where available) and mean MIS values were calculated for the different acquisition durations.
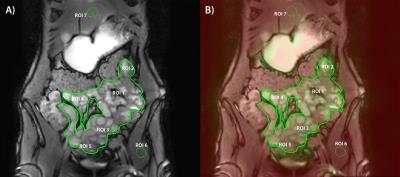
Motility analysis: For this study, seven ROIs were drawn. The first ROI is a global ROI including all the small bowel, the other ROIs are smaller, local ROIs (fig. 1). The calculated mean MIS within each ROI is plotted against the temporal resolution and scan duration for visualization of the robustness of the motility measure.
Results
Fig. 2 shows a dynamic MRI scan with a temporal resolution of 10 fps and a duration of 20 sec. It visualizes the bowel motility that is quantified using the mean motility index score (MIS). Fig. 3 shows the mean MIS values for the global small bowel ROIs in all volunteers at different temporal resolutions (A) and the quadrant ROIs (B) calculated at different temporal resolutions. Both figures show a stabilization of the mean MIS at a temporal resolution of 1 fps. Fig. 4 shows the mean MIS at different scan durations for the global ROI in all volunteers. Visually, the mean MIS appears to stabilize for scan durations of 10 sec. or more.Discussion / Conclusion
This study indicates the use of 1) a temporal resolution of at least 1 frame per second in small bowel motility imaging for both global and segmental motility analysis and 2) a scan duration of at least 10 seconds for consistent motility observations.Acknowledgements
No acknowledgement found.References
1. Plumb et al. (2015). Magnetic resonance imaging-quantified small bowel motility is a sensitive marker of response to medical therapy in Crohn's disease. Aliment Pharmacol Ther. 42(3):343-55.
2. Hahnemann et al. (2015). Quantitative assessment of small bowel motility in patients with Crohn's disease using dynamic MRI. Neurogastroenterol Motil. 27(6):841-8.
3. Menys et al. (2016) Comparative quantitative assessment of global small bowel motility using magnetic resonance imaging in chronic intestinal pseudo-obstruction and healthy controls. Neurogastroenterol Motil. (3):376-83.
4. F. Odille et al. (2012). Quantitative Assessment of Small Bowel Motility by Nonrigid Registration of Dynamic MR Images. Magn Reson Med. 68(3):783-93.
5. Menys et al. (2013). Global small bowel motility: assessment with dynamic MR imaging. Radiology. 269(2):443-50.
6. van der Paardt et al. (2014). Noninvasive automated motion assessment of intestinal motility by continuously tagged MR imaging. J Magn Reson Imaging. 39(1):9-16.
7. Bickelhaupt et al. (2014). Software-assisted small bowel motility analysis using free-breathing MRI: feasibility study. J Magn Reson Imaging. 39(1):17-23.
8. Akerman et al. (2016). Computational Postprocessing Quantification of Small Bowel Motility Using Magnetic Resonance Images in Clinical Practice: An Initial Experience. J Magn Reson Imaging. 44(2):277-87.
Figures