4981
PET/MRI for rectal cancer staging: Longer PET acquisition times result in increased identification of nodal metastatic disease.1Department of Radiology & Biomedical Imaging, University of California, San Francisco, San Francisco, CA, United States, 2Gastrointestinal Oncology, The UCSF Helen Diller Family Comprehensive Cancer Center, University of California, San Francisco, San Francisco, CA, 3Colorectal Surgery, University of California, San Francisco, San Francisco
Synopsis
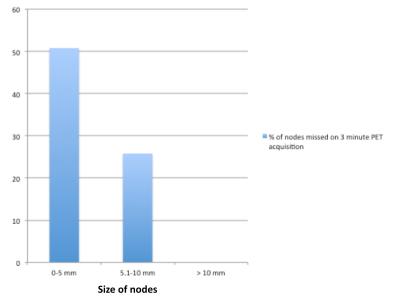
Rectal cancer nodal staging guides the decision to whether neo-adjuvant chemoradiation is needed prior to surgical resection and is a predictor of survival and recurrence. However, staging based on size and morphologic criteria alone is limited. Our data suggests that increased PET acquisition times with PET/MRI increases the identification of nodal metastatic disease in rectal cancer, particularly in small nodes sized 5 mm or less.
Purpose
PET/MRI has been suggested to be an optimal staging modality for rectal cancer, given its ability to stage the primary tumor as well as nodal staging. Nodal disease is a strong independent predictor of survival and recurrence in rectal cancer (1). Patients with N2 disease have a higher risk of local recurrence than those with NO or N1 disease (2). Therefore, accurate staging is essential for appropriate determination of rectal cancer surgical treatment and need for neo-adjuvant therapy. Given the limitation of staging based on nodal size and morphologic criteria alone, PET/MRI may provide a more accurate modality due to the high spatial resolution of MRI and the functional/metabolic information from PET (3). We aimed to determine whether longer PET acquisition times in the pelvis for PET/MRI identify more rectal cancer nodal metastases than the standard 3 minute whole body acquisition.Methods
22 patients who had biopsy proven rectal cancer were imaged using a simultaneous 3.0T time-of-flight PETMRI (Signa, GE Healthcare). Patients were imaged using a pelvic bed acquisition (15 minutes of PET acquisition) concurrent with a dedicated rectal MRI, and a whole body MRI using 3 minutes of PET acquisition at each bed. Nodes were identified on the 15 minute PET acquisition, the 3 minute PET acquisition, and then confirmed on the small field of view, high resolution T2 weighted sequences. Nodal staging was then calculated using the AJCC criteria.Results
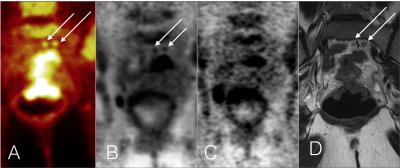
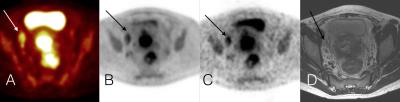
22 patients were imaged, 11 men and 11 women with a total of 29 studies. 17 patients were seen at initial staging and 5 at recurrence. There were a total of 94 nodes identified. All nodes on PET had an MRI correlate on T2 weighted imaging. Of the 94 nodes, 37 (39.4%) were seen only on the dedicated 15 minute pelvic PET acquisition. 57 nodes 5 mm or less were seen on PET with 29 detected only on the 15 minute acquisition and 28 seen on both acquisition times. 31 nodes sized 5.1 mm -10 mm were identified by PET, 8 seen only at the 15 minute acquisition and 23 seen on both. There were 6 nodes sized greater than 10 mm. All nodes greater than 10 cm were seen on both PET acquisitions. Of the 17 patient’s seen at initial staging, 11 were upgraded as a result, (64.7%), 10 from N1 to N2 and 1 from N0 to N1. Of the 29 total studies, 17 were upgraded (58.6%), 15 from N1 to N2 and 2 from N0 to N1.Discussion
Longer PET acquisition times increase the detection sensitivity for nodal disease. In the setting on simultaneous PET/MRI, additional PET imaging time is available due to the simultaneous MRI acquisition. In particular this is relevant for small nodes that may be negative by both MRI and PET, impacting the decision as to whether neoadjuvant chemoradiation is required prior to surgical resection. However, one must also consider that the increased sensitivity of the longer PET acquisition time may result in increased false positives, particularly in the post-treatment population, as not every node that is metabolically active on the 15 minute acquisition represents metastatic disease. Our data is limited as no nodal pathologic correlation was obtained for the nodal disease. Further testing, with more observers and definitive radiologic-pathologic correlation is necessary to confirm the true clinical utility of the longer PET/MRI acquisition times.Conclusion
PET/MRI with longer PET acquisition times results in an increased percentage of perirectal nodes that demonstrate uptake.Acknowledgements
References
(1)Koh DM, Brown G, Husband, JE. Nodal staging in rectal cancer. Abdominal Imaging (2006) 31(6): 652-9
(2)Moran MR, James EC, Rothenberger DA, Goldberg SM. Prognostic value of positive lymph nodes in rectal cancer. Dis Colon Rectum 35:579–581
(3) Fraum TJ, Owen JW, Fowler KJ. Beyond Histologic Staging: Emerging Imaging Strategies in Colorectal Cancer with Special Focus on Magnetic Resonance Imaging. Clinics in Colon and Rectal Surgery 2016; 29(03): 205-215
Figures