4980
Dynamic contrast enhanced MR imaging for therapeutic response assessment after neoadjuvant Chemoradiotherapy in patient with local advanced rectal cancer1Shanxi Province Tumor Hospital, Taiyuan, People's Republic of China, 2GE Healthcare China
Synopsis
The pre-CRT Ktrans value and the percentage decrease in the Ktrans after CRT could be helpful to predict good therapeutic response to CRT for LARC. This may allow for personalized treatment-options in rectal cancer patients.
Purposes
Over the past decades, great changes for the treatment of patients with locally advanced rectal cancer (LARC) has shifted from surgery toward neoadjuvant chemoradiotherapy (CRT), with the choice of further therapy depending on the degree of response to CRT(1-2). Patient selection for organ-sparing treatment after good or complete response to CRT is challenging, highlighting the need for accurate assessment of tumor response to CRT (3-4). Therefore, the purpose of our study was to determine the usefulness of the perfusion parameters derived from dynamic contrast enhanced magnetic resonance imaging (DCE-MRI) for assessing the therapeutic response to neoadjuvant CRT for LARC.
methods:
This retrospective study was approved by our institutional review board and written informed consent was waived. 43 patients with LARC underwent CRT and subsequent surgery, were enrolled in this study. All patient underwent pre- and post-CRT DCE-MRI at 3.0 T scanner (Achieva; Philips Healthcare, Best, The Netherlands) with 8-channel phased array torso coils. For DCE-MRI parameters, the volume transfer constant between blood plasma and extracellular/extravascular space (EES) (Ktrans, min-1), rate constant between EES and blood plasma (Kep, min-1), volume of EES space per unit volume of tissue (Ve) were measured for every tumor before and after CRT, using the noncommercial software, Omnikinetics (GE Healthcare, Beijing, China) with the two-compartment Extended Tofts model. Those perfusion parameters were compared not only between responder group (TRG1-2) and the non-responder group (TRG3-5), but also pre- and post-CRT in each group.results
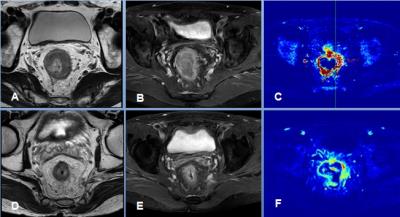
Eleven patients (25.6 %) were classified as responders, while 32 subjects (74.4 %) were considered as non-responders. Before CRT, the mean tumour Ktrans in the responder group was significantly higher than that in the non-responder group (P=0.015), but there was no significant difference for post-CRT Ktrans between these two groups (Table1).The percentage difference between pre- and post-CRT Ktrans in the responder group was significantly higher than that in the non-responder group (36%, 15%, respectively, P=0.005) (Figure1). However, none of the other parameters (Keq or Ve) showed significant differences neither pre- nor post-CRT.Discussion and Conclusion:
The pre-CRT Ktrans value and the percentage decrease in the Ktrans after CRT could be helpful to predict good therapeutic response to CRT for LARC. This may allow for personalized treatment-options in rectal cancer patients.Acknowledgements
NO.References
1. Maas M, Nelemans PJ, Valentini V, et al. Long-term outcome in patients with a pathological complete response after chemoradiation for rectal cancer: a pooled analysis of individual patient data. Lancet Oncol 2010;11(9):835–844.
2. O’Neill BD, Brown G, Heald RJ, Cunningham D, Tait DM. Non-operative treatment after neoadjuvant chemoradiotherapy for rectal cancer. Lancet Oncol 2007;8(7):625–633.
3. Maas M, Beets-Tan RG, Lambregts DM, et al. Wait-and-see policy for clinical complete responders after chemoradiation for rectal cancer. J Clin Oncol 2011;29:4633–4640.
4. Allaix ME, Fichera A. Modern rectal cancer multidisciplinary treatment: the role of radiation and surgery. Ann Surg Oncol 2013;20:2921–2928.