4969
Magnetization transfer MRI for evaluating bowel fibrosis and inflammation in patients with stricturing Crohn’s diseaseXuehua Li1, Zhuangnian Fang1, Siyun Huang1, Li Huang1, Zhongwei Zhang2, Xu Yan3, Xiaolei Zhu4, Jinjiang Lin1, Mengchen Zhang1, Mengjie Jiang1, Shiting Feng1, Canhui Sun1, and Ziping Li1
1Department of Radiology, The First Affiliated Hospital of Sun Yat-Sen University, Guangzhou, People's Republic of China, 2Department of Biomedical Engineering, Cancer Biology and Radiology, Wake Forest School of Medicine, NC, United States, 3MR Collaboration NE Asia, Siemens Healthcare, Shanghai, People's Republic of China, 4MR Scientific Marketing NE Asia, Siemens Healthcare, Guangzhou, People's Republic of China
Synopsis
This study aimed to assess the efficacy of Magnetization Transfer MRI (MTI) for evaluating bowel fibrosis and inflammation in patients with stricturing Crohn’s Disease (CD). Bowel wall MTR with normalization to skeletal muscle was calculated and correlated to histologic fibrosis and inflammation as well as amount of type I collagen and vessel density. The results showed that normalized MTRs correlated with histologic fibrosis and type I collagen scores, but did not correlate with inflammation scores or vessel densities. Thus, MTI can accurately detect and distinguish varying degrees of bowel fibrosis with or without coexisting inflammation in human CD.
Introduction/Purpose
Crohn’s disease (CD) is a chronic inflammatory bowel disease characterized by segmental and transmural bowel wall inflammation that often progresses to fibrosis with intestinal strictures and obstruction. Differentiating the fibrostenotic from the inflammatory component of strictures is clinically important; however, it is still insufficiently evaluated by using clinical response, conventional magnetic resonance imaging (MRI), or computed tomography. Recently, magnetization transfer MRI (MTI) has shown potential in detecting bowel fibrosis in CD. The objective of this study was to assess the efficacy of MTI for differentiating fibrotic from inflammatory stricture and for grading of bowel fibrosis in patients with CD, compared with surgical histopathology as the reference standard.Methods
MTI
data of 12 patients (4 men, 8 women; mean age: 32.9 ± 9.2 years) with known CD
were acquired using a 3T MR system (MAGNETOM Trio, Siemens Healthcare,
Erlangen, Germany), and were analyzed before elective surgery. MTI was
performed using two breath-held axial 2D gradient-echo sequences with and
without application of a 1.2 kHz off-resonant pre-saturation-pulse. Bowel wall
magnetization transfer ratio (MTR) with normalization to skeletal muscle was
calculated, and the region-by-region correlation between MTR and histologic
degree of fibrosis / inflammation, as well as amount of type I collagen and
vessel density from the surgical specimen, was performed.Results
Normalized MTRs strongly correlated with histologic degree of fibrosis (r=0.711) and moderately correlated with type I collagen scores (r=0.362), but did not correlate with inflammation scores (r=0.177) or vessel densities (r=0.184). Normalized MTRs of 59 examined fibrotic bowel walls were significantly higher compared to 61 non-fibrotic bowel walls (P<0.001). Significant differences in normalized MTRs were also shown among mildly, moderately and severely fibrotic walls (all P<0.05). Receiver operating characteristics (ROC) curve analysis showed high accuracy of normalized MTRs with an area under ROC curve of 0.920 (P<0.001) for differentiating fibrotic and non-fibrotic bowel walls. Using normalized MTR of 0.62 as a cutoff value, the diagnostic sensitivity and specificity for differentiating between fibrotic and non-fibrotic bowel walls were 88.10% and 86.90%, respectively.Discussion
In our study, the normalized MTR increased with the severity of bowel fibrosis. The ability of MTI to detect and further stratify bowel fibrosis regarding disease severity could assist in surveillance of the natural progression of CD. Meanwhile, MTI was sensitive to the changes in bowel fibrosis but not to that of inflammation. In our study, this feature demonstrates the reliability of MTI for detecting the presence and severity of bowel fibrosis. Moreover, we found a fair correlation between normalized MTR and type I collagen, another hallmark feature of intestinal fibrosis, which has previously been speculated to be nonlinear.Conclusions
MTI can accurately detect and distinguish varying degrees of bowel fibrosis with or without coexisting inflammation, which can be considered as a potential tool for treatment planning and surveillance of CD progression.Acknowledgements
No acknowledgement found.References
No reference found.Figures
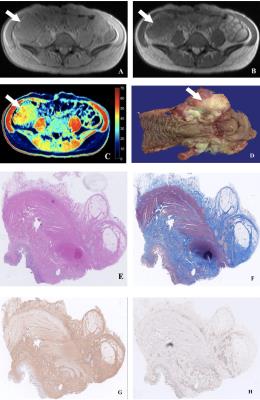
Figure
1. Axial
MTI without (A) and with MT (B) pulse and color MTR map (C) demonstrate high MT
effect of ileocecum (arrows) corresponding to thickened bowel wall with
gray-white cut surface on macroscopic specimen (D). Histologic evaluation shows
moderate inflammation (E), marked transmural fibrosis (F) and type I collagen (G), and abundant vessels (H)
in the affected bowel wall.
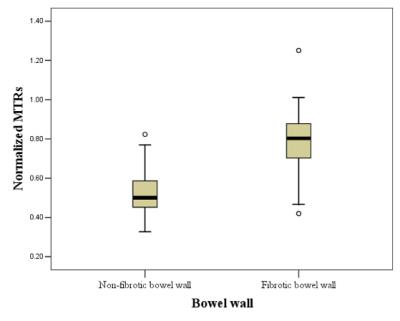
Figure
2. Normalized
MTRs of fibrotic bowel walls were significantly higher compared to non-fibrotic
bowel walls.
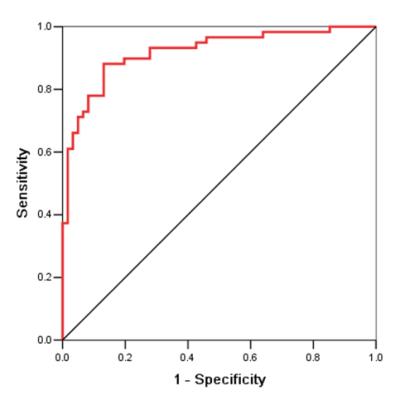
Figure
3. ROC curve demonstrates high accuracy of normalized MTRs with
an AUC of 0.920 for differentiating fibrotic
and non-fibrotic bowel walls.