4962
Comparison of Radiologist Perception of Image Quality of Advanced Diffusion vs. RESOLVE Diffusion1Radiology and Biomedical Imaging, UCSF, San Francisco, CA, United States, 2Siemens Medical Solutions
Synopsis
In order to gain acceptance of DWI in the clinical setting, consistent high image quality with minimal breast distortion is required. Although time of acquisition is slightly longer for the RESOLVE compared with the advanced diffusion sequence, the benefits of improved image quality, particularly with respect to image distortion and phase ghosting are preferred by clinical breast imaging radiologists based on this reader study. The theoretical benefits of using readout-segmented diffusion imaging technique in RESOLVE to improve image quality can be realized in a routine clinical practice.
Background
Addition of diffusion weighted imaging (DWI) to routine clinical breast MRI protocols provides complementary information to DCE-MRI for lesion characterization and can potentially improve the specificity of breast MRI. Numerous studies have demonstrated restricted water diffusion in breast malignancies and significant differences in ADC values of benign and malignant lesions (1-3). However, variable image quality of breast DWI due to the frequency of inadequate fat suppression, image distortion and other artifacts has limited clinical adoption of DWI in breast imaging. In order to gain acceptance of DWI in the clinical setting, consistent high image quality with minimal breast distortion is required.Purpose
The purpose of this study was to compare radiologist perception of DWI image quality on advanced diffusion & RESOLVE diffusion sequences acquired under routine clinical conditions.Methods
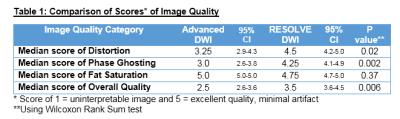
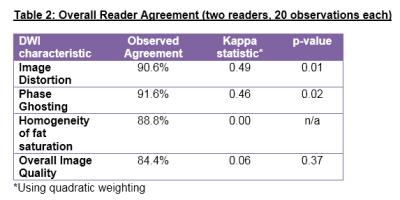
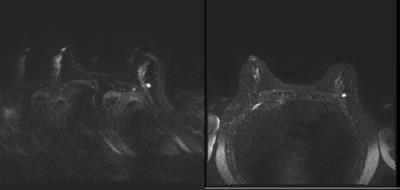
This was an IRB-approved, HIPAA-compliant study. During the month of September, 2015 we transitioned from the Advanced (single shot) DWI sequence to the RESOLVE (epi) DWI sequence as part of our routine clinical breast MR protocol. The first 10 consecutive clinical breast MR exams during the month preceding the transition and during the month following the protocol transition were identified for a total of 20 exams: 10 Advanced DWI and 10 RESOLVE DWI. Scan parameters for the advanced diffusion sequence were: TA 5:35min, 1.8x1.8x2.4 mm, 43 transverse slices, BW: 18.8Hz, TR/TE/FL: 8000.0/ 82.4/180, NEX 2, b value = 0, 100, 600, 800 sec/ mm^2. Scan parameters for the RESOLVE sequence were TA: 6:03min; 1.6x1.6.x2mm, 56 transverse slices, TE/TR=80/9800 msec, Ipat(GRAPPA)2, Echo spacing 0.32msec, b value = 0 and 800 sec/mm^2. Two fellowship trained breast imaging radiologists independently evaluated image quality of the diffusion weighted sequences (b0 and b800) on anonymized images obtained at nipple level with the corresponding axial T2 TSE and axial VIBE pre-contrast images available for anatomic reference. Readers were asked to rate image distortion, phase ghosting, homogeneity of fat suppression, and overall image quality of the diffusion images using a 5-point scale where 1 represents poor (uninterpretable) image quality with significant artifact (Figure 1) and 5 represents excellent image quality with almost no artifact. Each reader evaluated the cases in a different randomized order, blinded to type of diffusion sequence. Reader scores were tabulated and image quality ratings for the two sequences compared using the Wilcoxon rank sum test with p<0.05 considered significant. Reader agreement for each type of diffusion sequence and for overall image quality were also evaluated.Results
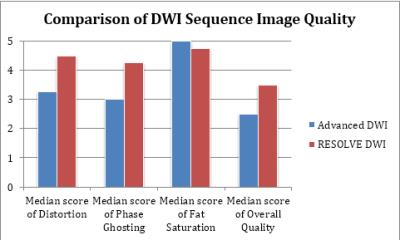
RESOLVE DWI scored significantly higher for image quality overall as compared to Advance DWI (medians [95% CI]: 3.5 [3.6-4.5] vs. 2.5 [2.6-3.6], p= 0.006). RESOLVE DWI also scored significantly higher for image distortion and phase ghosting (Figure 2, Table 1). Both sequences scored well in terms of fat saturation with no significant differences (medians [95% CI]: 4.75 [4.7-5.0] vs. 5.0 [5.0-5.0], p = 0.37). Although the observed inter-reader agreement between two readers was 84-91% and significantly higher than the expected agreement, the Kappa quadratic score was poor to moderate, indicating high inter-reader variability (Table 2). This lower kappa may be explained by the fact that the reader scores clustered toward the higher end of the scale rather than being evenly distributed from 1 to 5. Overall, this may be a positive result because it indicates reasonable image quality for both diffusion sequences.Conclusion
Although time of acquisition is slightly longer for the RESOLVE compared with advanced diffusion sequence, the benefits of improved image quality, particularly with respect to image distortion and phase ghosting are preferred by clinical breast imaging radiologists.Acknowledgements
No acknowledgement found.References
1. Ei Khouli RH, Jacobs MA, Mezban SD, et al. Diffusion-weighted imaging improves the diagnostic accuracy of conventional 3.0-T breast MR imaging. Radiology 2010;256(1):64-73.
2. Partridge SC, Rahbar H, Murthy R, et al. Improved diagnostic accuracy of breast MRI through combined apparent diffusion coefficients and dynamic contrast-enhanced kinetics. Magn Reson Med 2011;65(6):1759-1767.
3. Partridge SC, DeMartini WB, Kurland BF, Eby PR, White SW, Lehman CD. Quantitative diffusion-weighted imaging as an adjunct to conventional breast MRI for improved positive predictive value. AJR Am J Roentgenol 2009;193(6):1716-1722.
Figures