4958
Rectal perfusion parameters normalized to tumour free rectal wall can predict complete pathological response to neoadjuvant chemoradiotherapy.1Radiology, Medanta Hospital Gurgaon, Gurgaon, India, 2Radiology, Medanta Hospital, India
Synopsis
The aim of this study was to evaluate absolute and normalized change in qualitative and semi quantitative perfusion parameters in predicting complete pathological response to CRT. Perfusion parameters of Pre and post treatment imaging of histopathologically proven 10 patients with rectal cancer who had complete response and complete absence of tumour on histopathology following complete treatment ( Group 1) were compared with 10 patients with residual tumour on histopathology following treatment (Group 2). The two groups were matched for T stage of tumour. Semiquantittaive perfusion MRI parameters (Ktrans, Kep, Ve, IAUC; Toft model) were quantified by manually delineating a region of interest in the upper, mid and lower third of tumour at least 1cm square, in addition similar parameters were obtained from the normal rectal wall atleast 1cm away from the potential resection margin, absolute as well as values normalized values to the perfusion in the normal rectal wall were evaluated. Qualitative perfusion parameters were also assessed (wash in, wash out, TTP, AT, PEI, iAUC). After CRT, all patients underwent complete surgical resection and the surgical specimen served as the gold standard. Difference in absolute and normalized qualitative parameters were compared within each group using paired t-test and between each group using ANOVA. Washin, Washout, PEI, Ktrans, IAUC in the complete pathological responders when normalized to the adjacent normal rectal wall showed ratio’s approaching near 1 suggesting that rectal perfusion returns similar to the adjacent normal rectal wall in complete pathological responders. The difference in the normalized values in the responders and non responders was statistically significant. Within group change in absolute mean values in the responders and non responders was not statistically significant. Perfusion parameters can be used in predicting response to treatment, when normalised to the adjacent normal rectal wall.
PURPOSE
Quantitative perfusion DCE-MRI has been extensively explored for evaluation of microvascular perfusion and permeability change of rectal cancer compared with normal rectal wall 1. It is known that tumours with high pre-CRT(chemoradiotherapy) K (trans) values tended to respond favourably to CRT, particularly in terms of down-staging criteria 1,2. However quantitative cut off values which can predict complete response to treatment are lacking in literature 3. The aim of this study was to evaluate absolute and normalized change in qualitative and semi quantitative perfusion parameters in predicting complete pathological response to CRT.METHODS
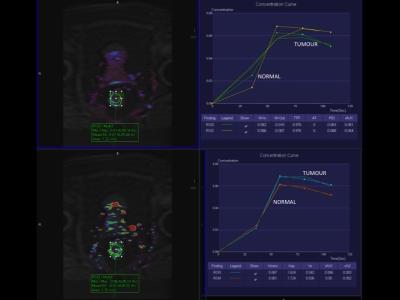
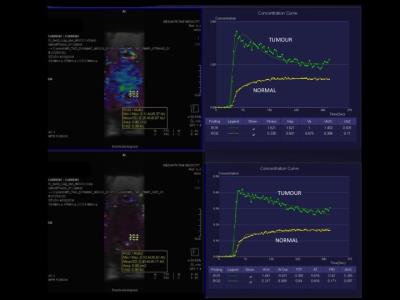
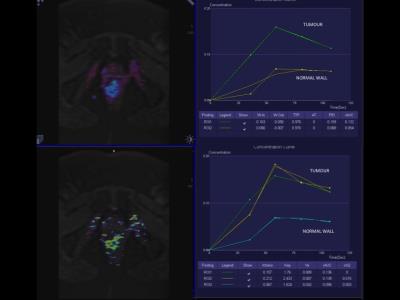
Perfusion parameters of Pre and post treatment imaging of histopathologically proven 10 patients with rectal cancer who had complete response and complete absence of tumour on histopathology following complete treatment ( Group 1) were compared with 10 patients with residual tumour on histopathology following treatment (Group 2). The two groups were matched for T stage of tumour. Treatment protocol consisted of neoadjuvant chemoradiotherapy with oxaliplatin and 5-fluorouracile. Semiquantittaive perfusion MRI parameters (Ktrans, Kep, Ve, IAUC; Toft model) were quantified by manually delineating a region of interest in the upper, mid and lower third of tumour at least 1cm square, in addition similar parameters were obtained from the normal rectal wall atleast 1cm away from the potential resection margin, absolute as well as values normalized values to the perfusion in the normal rectal wall were evaluated. Qualitative perfusion parameters were also assessed (wash in, wash out, TTP, AT, PEI, iAUC). In addition 10 normal patients without any malignant rectal pathology were also included. All the images were anonymised and analyzed at Tissue 4D post-processing workstation (Siemens AG) for post-processing. Colour coded perfusion maps were co-registered on the anatomical T2W images for ROI measurement. Imaging protocol included three orthogonal (axial/coronal/sagital) high-resolution T2-weighted turbo spin-echo (TSE) scans. DCE MRI was performed using a free-breathing T1-weighted three-dimensional (3D) spoiled gradient echo fat low-angle shot (FLASH) sequence with fat suppression on the sagittal plane. The protocol for the T1 map included a T1-weighted sequence with flip angle of 2 and 15 0. Dynamic T1-weighted images were obtained with temporal resolution of 1.5-1.6 seconds, at the same field of view and matrix as those of the T1 map protocol. Gadoterate Meglumine (Dotarem, Guerbet) 0.2 mL/kg (0.1 mmol/kg) IV bolus was infused at rate of 2 mL/second with a saline chase of 20 mL After CRT, all patients underwent complete surgical resection and the surgical specimen served as the gold standard. Difference in absolute and normalized qualitative parameters were compared within each group using paired t-test and between each group using ANOVA. ROC was performed to generate a cut off value of possibleRESULTS
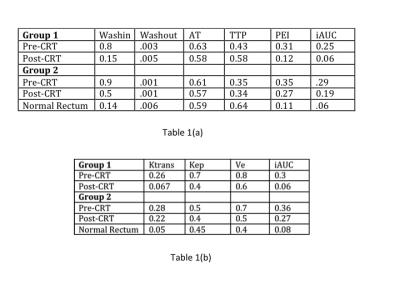
Table 1 shows mean absolute qualitative (Table 1a) and semi-quantitative values in the two groups before and following treatment (Table 1b). Table 2 ( qualitative-2a, semi-quantitative 2b) shows normalized value (ratio of tumor to normal rectal wall) of the two groups before and following treatment. Washin, Washout, PEI, Ktrans, IAUC in the complete pathological responders when normalized to the adjacent normal rectal wall showed ratio’s approaching near 1 suggesting that rectal perfusion returns similar to the adjacent normal rectal wall in complete pathological responders. The difference in the normalized values in the responders and non responders was statistically significant. Within group change in absolute mean values in the responders and non responders was not statistically significant.CONCLUSION
Perfusion parameters can be used in predicting response to treatment, when normalised to the adjacent normal rectal wall.DISCUSSION
While most studies have evaluated serial change in values none have come up with absolute change which can predict complete pathological response. This is very important since complete pathological response in patients with low rectal cancer can be used for doing sphincter sparing surgery. Perfusion MRI has potential to be considered as a surrogate marker of complete pathological response and close follow-up, patients can be monitored, thus avoiding immediate surgery and still have good oncological outcome. This conservative approach is particular attractive for elderly and medically unfit patientsAcknowledgements
No acknowledgement found.References
1. Martens MH1, Subhani S2, Heijnen LA et al Can perfusion MRI predict response to preoperative treatment in rectal cancer? Radiother Oncol. 2015 Feb;114(2):218-23.
2. Hötker AM1, Garcia-Aguilar J, Gollub MJ. Multiparametric MRI of rectal cancer in the assessment of response to therapy: a systematic review. Dis Colon Rectum. 2014 Jun;57(6):790-9.
3. Lim JS1, Kim D, Baek SE, Perfusion MRI for the prediction of treatment response after preoperative chemoradiotherapy in locally advanced rectal cancer. Eur Radiol. 2012 Aug;22(8):1693-700.
Figures