4957
Poor enhancement of colorectal liver metastases on delayed phase gadobutrol enhanced MRI may be related to increased number of APC mutations1Medical Imaging, Sunnybrook Health Sciences Centre, University of Toronto, Toronto, ON, Canada, 2Sunnybrook Research Institute, 3Sunnybrook Health Sciences Centre
Synopsis
We recently demonstrated that delayed enhancement of colorectal liver metastases (CRLM) on gadobutrol-enhanced MRI is associated with long-term survival. We performed a hypothesis-generating pilot study to determine whether delayed enhancement on MRI is related to the number and types of genetic mutations. There were a greater number of somatic APC mutations in hypoenhancing tumors compared to isoenhancing tumors or hyperenhancing tumors (N=15, p=0.013). There was no difference in the number of germline mutations or number of overall somatic mutations among MRI groups. Poor enhancement of CRLM on delayed phase gadobutrol-enhanced MRI may correlate with increasing number of somatic APC mutations.
Introduction
Colorectal cancer is the second leading cause of cancer deaths in the United States (1). Most deaths are related to metastatic disease and the liver is the most common site for metastases. There have been recent advances in surgery and chemotherapies (including targeted chemotherapeutic agents) that have significant improved outcomes for patients (2-3). However, the survival of patients remains quite variable, likely due to heterogeneity in the biology and genetics of individual tumors (4-5). We recently demonstrated that delayed enhancement of colorectal liver metastases (CRLM) on gadobutrol-enhanced MRI is associated with long-term survival (6). Understanding the biological mechanisms for this differential in survival may also help us risk-stratify patients, optimize therapy regimens for individual patients, and determine new potential targets for chemotherapy. The goal of this study was to determine whether delayed enhancement of CRLM is related to the number and types of genetic mutations within tumors.Methods
We performed a retrospective, IRB-approved, pilot study on 15 patients who had received a preoperative gadobutrol-enhanced liver MRI prior to liver resection for CRLM.
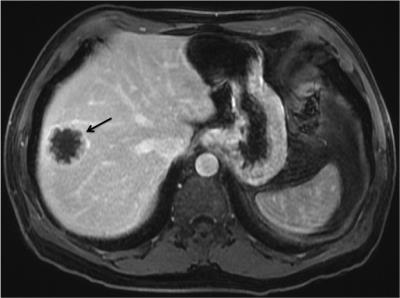
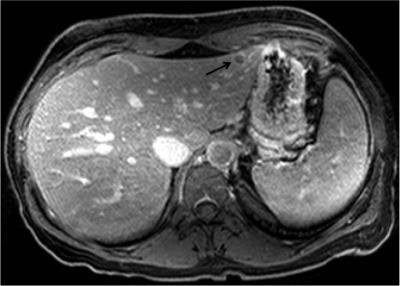
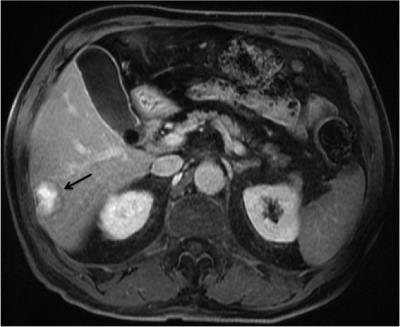
As part of the contrast-enhanced series, delayed 3D Axial T1 imaging is routinely performed approximately 10-minutes post-contrast injection of an intravenous dose of gadobutrol, at 0.1mL/kg body mass up to 10mL at 1.0mmol/mL. All studies were performed on 1.5T (GE Twinspeed, TR~4.5, TE~2.2, Flip Angle~15, Slice thickness=5mm, Spacing=2.5mm, FOV=380mm, Matrix = 320x192) or 3.0T (Philips Achieva, TR~3.0, TE~1.4, Flip Angle~10, Slice thickness=3mm, Spacing=1.5mm, FOV~380, Matrix ~ 250x250) magnets with an eight-channel body phased array coil covering the entire liver. We measured the contrast-to-noise ratio of each CRLM on 10-minute delayed phase gadobutrol-enhanced MRI and divided the patients into hyperenhancing (CNR > 10), isoenhancing (-10<CNR<10), and hypoenhancing (CNR < -10).
We obtained cores of liver metastases and normal liver tissue from post-hepatectomy pathology specimens in the same patients and performed deep sequencing using Ion AmpliSeq Cancer Hotspot Panel to survey hotspot regions of 50 oncogenes and tumor suppressor genes (ThermoFisher Scientific). For samples of normal tissue, we performed sequencing with 100-fold coverage for germline mutations. For tumor samples, we performed sequencing with 1000-fold coverage for somatic mutations.
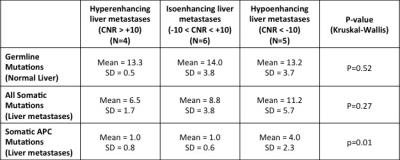
We determined the number of germline mutations, somatic mutations, and somatic APC mutations for each patient and compared this between MRI groups using the Kruskal-Wallis test.
Results
There were 4 patients with hyperenhancing tumors, 6 patients with isoenhancing tumors, and 5 patients with hypoenhancing tumors. There was no difference in the number of germline mutations in the normal liver between MRI groups (p=0.517). There was a trend towards increasing number of somatic mutations with hypoenhancing tumors (mean of 11.2 mutations) compared with isoenhancing (mean of 8.8 mutations) and hyperenhancing tumors (mean of 6.5 mutations), which was not statistically significant (p=0.273). There was a greater number of somatic APC mutations with hypoenhancing tumors (mean of 4.0 mutations) compared with isoenhancing tumors (mean of 1.0 mutations) and hyperenhancing tumors (mean of 1.0 mutations) (p=0.013).Discussion
This hypothesis-generating pilot study provides preliminary evidence that poor enhancement of CRLM on delayed phase gadobutrol-enhanced MRI may correlate with an increasing number of somatic APC mutations. Larger studies are required to confirm our findings. Although other mutations (eg. KRAS, BRAF, TP53, etc.) may also be related to MRI findings, the frequency of these mutations was lower than with APC and our study was not powered to detect any differences. Other studies have determined that increasing number of APC mutations may be associated with worse prognosis (7).Conclusion
This study provides preliminary evidence that poor enhancement of CRLM on delayed phase gadobutrol-enhanced MRI may correlate with increasing number of somatic APC mutations.Acknowledgements
Thank you to Vivekanandan Thayalasuthan for his administrative support.References
(1) American Cancer Society. Cancer Facts & Figures 2016. Atlanta: American Cancer Society; 2016. Last accessed: November 6, 2016. Available online: http://www.cancer.org/acs/groups/content/@research/documents/document/acspc-047079.pdf
(2) Kanas GP, Taylor A, Primrose JN, Langeberg WJ, Kelsh MA, Mowat FS, et al. Survival after liver resection in metastatic colorectal cancer: review and meta-analysis of prognostic factors. Clin Epidemiol. 2012;4:283-301.
(3) Fakih MG. Metastatic colorectal cancer: current state and future directions. J Clin Oncol. 2015; 33:1809-1824.
(4) Gerlinger M, Rowan AJ, Horswell S, et al. Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N Engl J Med. 2012; 366(10):883-892.
(5) Watanabe T, Kobunai T, Yamamoto Y, et al. Heterogeneity of KRAS status may explain the subset of discordant KRAS status between primary and metastatic colorectal cancer. Dis Colon Rectum. 2011;54(9):1170-1178.
(6) Cheung HMC, Kim J, Hudson JM, Milot L. Hyperintensity on delayed-phase, gadobutrol-enhanced MRI is a significant predictor of survival in a nonsurgical population with colorectal liver metastases. Insights Imaging 2016; 7: 162. doi:10.1007/s13244-016-0475-8, [Online February 12, 2016].
(7) Schell MJ, Yang M, Teer JK, et al. A multigene mutation classification of 468 colorectal cancers reveals a prognostic role for APC. Nat Commun. 2016; 7:11743.
Figures